Articles / The new CPD – more pain but no gain, survey finds

0 hours
These are activities that expand general practice knowledge, skills and attitudes, related to your scope of practice.
0 hours
These are activities that require reflection on feedback about your work.
0 hours
These are activities that use your work data to ensure quality results.
These are activities that expand general practice knowledge, skills and attitudes, related to your scope of practice.
These are activities that require reflection on feedback about your work.
These are activities that use your work data to ensure quality results.
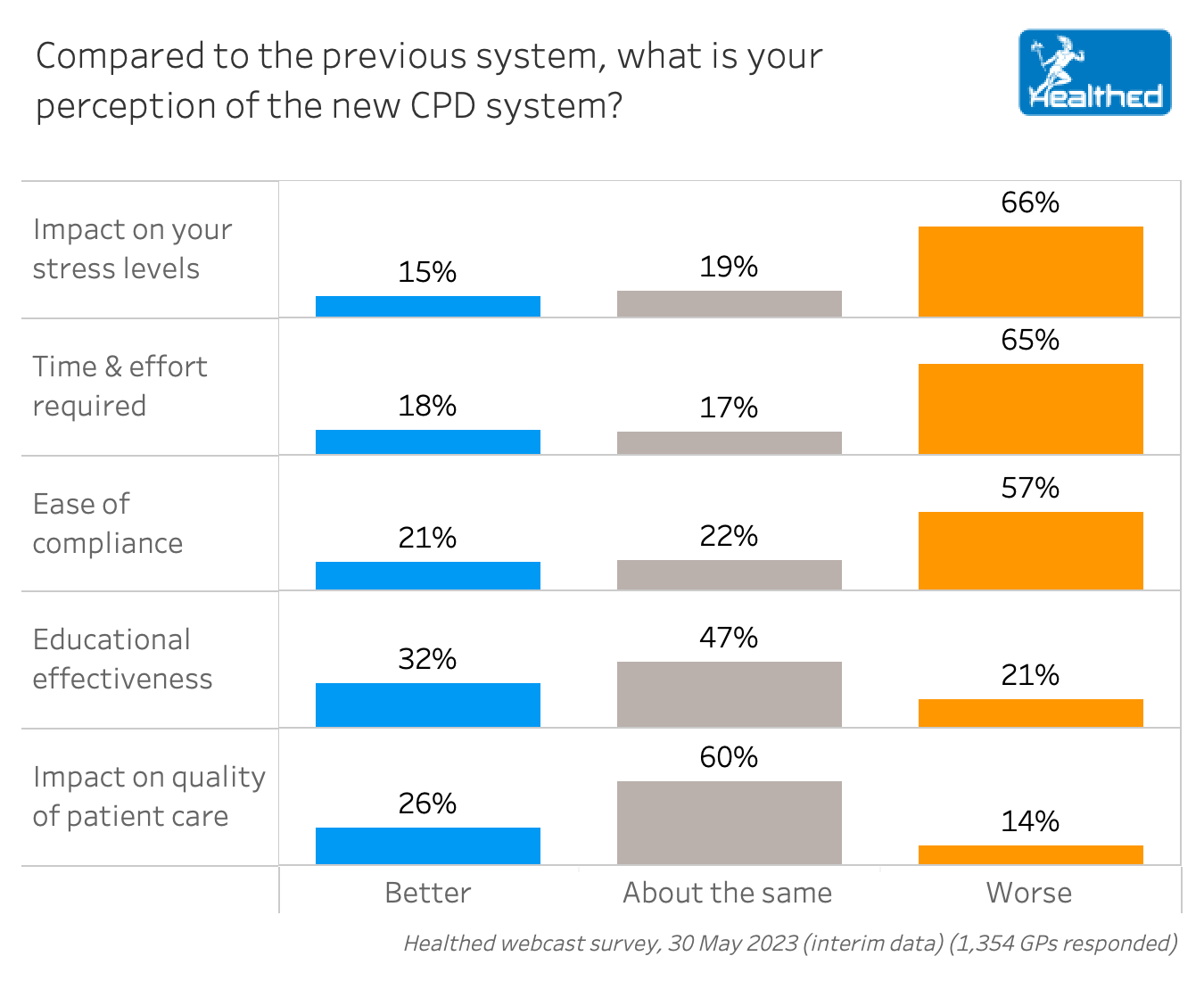
The new CPD program is more arduous, stressful and time-consuming than the previous system—and unlikely to result in improved patient care, a national survey of more than 1300 GPs suggests.
Two-thirds of GPs who responded to the survey said the new requirements had a negative impact on their stress levels and required more time and effort—while 68% could see no benefit in terms of educational effectiveness and 74% said the extra requirements would not translate to better patient care.
Dr Aniello Iannuzzi, chair of the Australian Doctors Federation, says doctors already have a duty of care to stay up-to-date and continually educate themselves, so the new CPD system just adds to counter-productive bureaucracy.
“As your survey highlights, the ever-increasing obligations, time and costs of CPD causes stress and confusion and therefore becomes a distraction away from the improvement of medical knowledge and skills,” Dr Iannuzzi said.
“The extra administrative burden therefore adds no value to the equation. Moreover it pushes up the cost of practising and takes valuable time and energy needed for patient care,” he said.
“It’s just becoming ticking boxes for the sake of doing it, and then you end up doing education that’s not relevant to you because you’ve got to satisfy these criteria.” – Dr Aniello Iannuzzi, chair of the Australian Doctors Federation
Dr Chris Irwin of the Australian GP Alliance also questioned the value of the new system.
“The problem with bureaucracy is that they need to change things not because it is better, but simply to justify their own existence,” Dr Irwin said.
“There is zero evidence that these CPD changes will improve patient care. If there is no evidence – why are we doing it? Would we as clinicians give patients a new treatment with zero evidence to back it up?” he continued.
“It is simply more pointless administrative load for doctors with zero evidence of improvement of patient care. GPs are already stressed and adding to that does not sound like an effective way to build a sustainable primary care health system.” – Dr Chris Irwin of the Australian GP Alliance
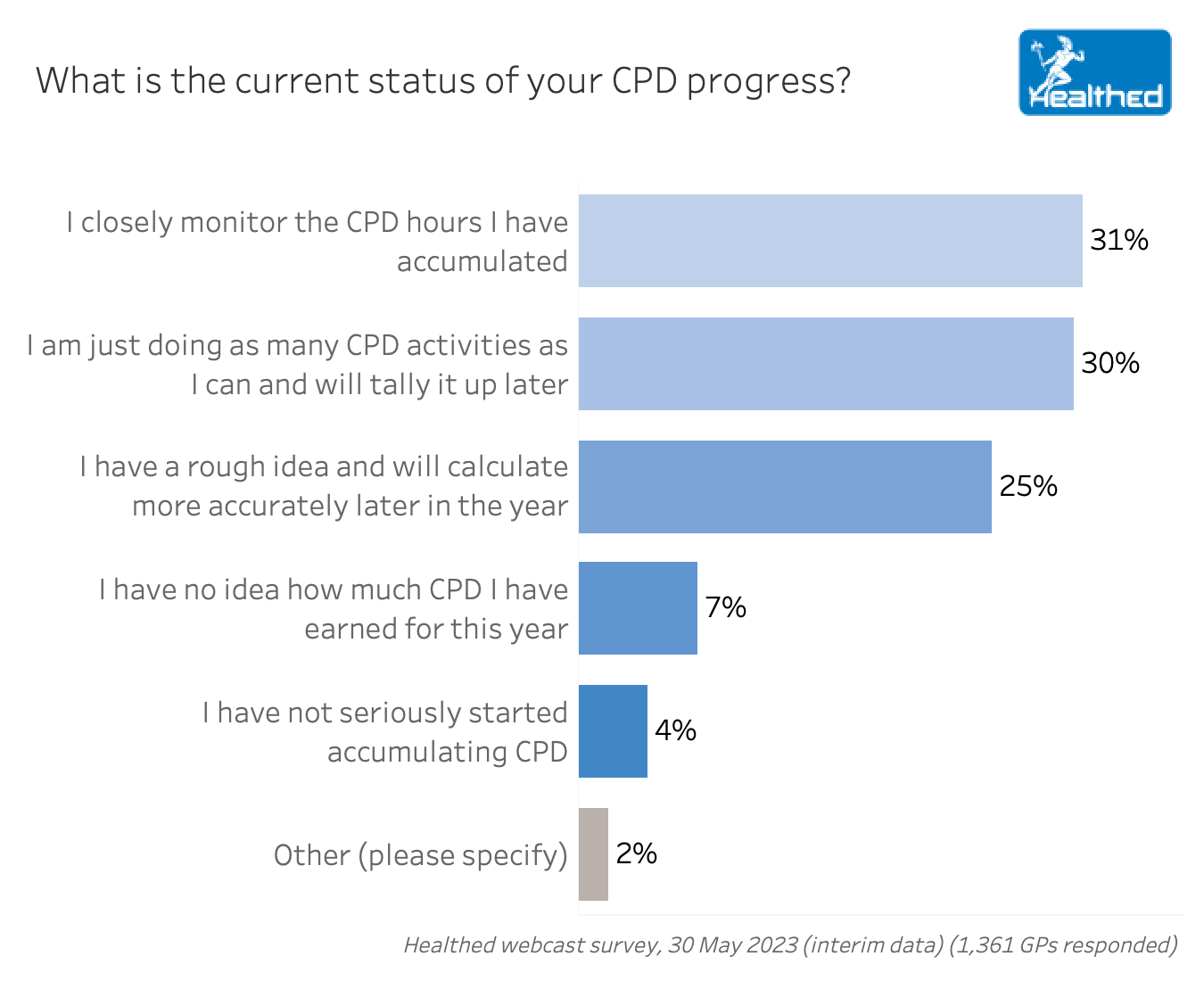
Close to one third of GPs (31%) said they are closely monitoring their CPD progress, while another 30% said they have a rough idea and will tally up their hours later. About one in ten GPs (11%) said they either haven’t started or don’t know how much CPD they have done this year.
Those GPs who are keeping a close eye on their CPD have completed an average of 31 hours so far.
Meanwhile, nearly half of GPs (48%) said they’ve yet to do their Personal Development Plan which was intended to be completed at the start of the year.
Additionally, more than one quarter of GPs (28%) said they don’t have time to fulfil the requirements, while 23% said they don’t understand the new system.
What your colleagues are saying
“I resent the ‘Measuring Outcomes’ bureau-speak, reminiscent of an episode of “Utopia”. Where is the evidence this will make bad doctors good, or good doctors better.”
“It seems a kick in the teeth as reward for 50 years dedicated service to my community. Despite my previous intention (and capability) to continue contributing in practice for another 2 years, this latest set of bureaucratic hoops to jump through may well be the last straw for me. I am sorry for my patients and for my already overloaded colleagues. One fewer GP- and one more to replace!”
“I learn based on my need…so the new changes in CPD requirements do not add any value to my learning, but require additional time and effort.”
“I always read and keep up to date and pursue topics as they arise in my practice – without necessarily following a formal assessment process.”
“Wasted clinician time recording activities that will have no useful impact on patient care”
“Instead of focusing on learning, far too much emphasis is placed on ‘self reflection’, and ticking boxes to gain points. And when it comes to providing additional comments, one ends up just providing what we think will placate any overseeing body.”
“What troubles me is the ‘secretarial duties’ now imposed on me – I am not a good ‘secretary’ and I am turned off by this aspect. I simply want to keep learning and applying the updated information in my clinician role.”

Vision and Driving Fitness: Key Insights for Health Practitioners

Role of Testosterone During Menopause – Evidence vs Hype

STIs – Common and Tricky Cases

RSV Prevention in Infants and Pregnant Women
Yes
No
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Notifications