Articles / CKD medical management – key updates

0 hours
These are activities that expand general practice knowledge, skills and attitudes, related to your scope of practice.
0.5 hours
These are activities that require reflection on feedback about your work.
0 hours
These are activities that use your work data to ensure quality results.
These are activities that expand general practice knowledge, skills and attitudes, related to your scope of practice.
These are activities that require reflection on feedback about your work.
These are activities that use your work data to ensure quality results.
Medications that can slow the progression of CKD by 15 years or more have recently been listed on the PBS, meaning for the first time, GPs have treatments they can prescribe for CKD regardless of a person’s comorbidities.
This means there’s now an imperative to assess and diagnose CKD earlier, and the Chronic Kidney Disease (CKD) Management in Primary Care handbook has been updated to reflect these and other significant advances over the last 18 months.
“This is the first in about 20 years that there’s been new medications available for CKD, and the first time that any treatment’s had a specific CKD listing,” says Breonny Robson, General Manager of Clinical and Research at Kidney Heath Australia, who has been involved in developing the last four editions of the handbook.
These include two sodium-glucose cotransporter-2 (SGLT2) inhibitors, and a non-steroidal MRA (more details below).
“These medications have the most benefit the earlier you prescribe them,” Ms Robson says.
“When you see someone with diabetes, or high blood pressure, you need to be thinking about kidneys. Because there’s meditation that you can prescribe that’s going to slow the progression. If you don’t diagnose someone, you can’t prescribe the medication.”
People can lose 90% of their kidney function before symptoms begin, and in Australia, 17% of individuals commence dialysis treatment within 90 days of referral to a renal unit – often because they are not detected until they reach kidney failure.
Early detection gives patients time to make positive lifestyle changes and consider treatment options that can help prevent further deterioration.
The Handbook includes an updated algorithm to improve detection and diagnosis of CKD.
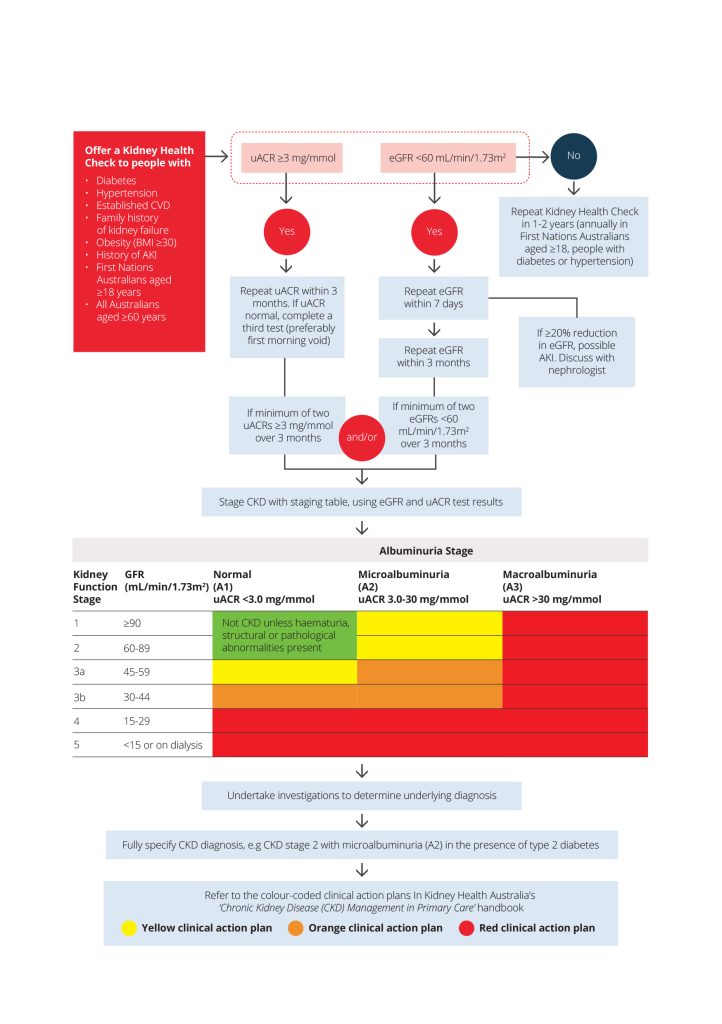
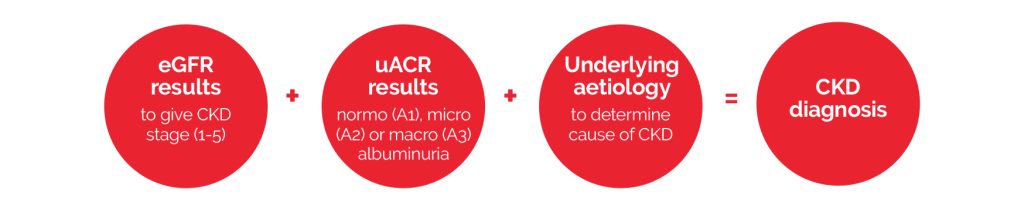
1. To diagnose CKD, you need eGFR results, uACR results, and information about underlying aetiology.
2. Once diagnosed, CKD should be staged using the colour coded staging table within the handbook. The staging table colours correspond to colour-coded action plans that outline the goals of management, frequency of review and treatment strategies related to the severity of CKD.
3. Remember to code the diagnosis in your practice software. This can help with medication management and flags the patient’s CKD status to other providers in the practice.
“Coding a CKD diagnosis in practice software is really important because then when they come to do medication management, that patients flagged as having CKD,” Ms Robson explains. “So if a pharmacist does a home medicine review, it’s flagged there that the person’s got CKD.”
Reduction of albuminuria is an essential goal of CKD treatment. Albuminuria is a key marker of kidney damage. There is robust evidence that albuminuria predicts both cardiovascular and kidney risk in people with CKD, and that reduction of albuminuria is renoprotective.
The CKD handbook recommends a target uACR reduction of at least 30% for all people with CKD and albuminuria.
While earlier handbooks focused on dose reduction and avoidance of nephrotoxic medications, the 5th edition contains specific advice on medications to initiate to slow CKD progression, reduce albuminuria and reduce cardiovascular risk, Ms Robson says.
To aid clinical decision-making, it introduces a step-by-step approach to treating patients with persistent macroalbuminuria.
1. Start an ACE inhibitor or ARB if they are not already using one for hypertension.
2. Up-titrate the ACE inhibitor or ARB to maximum tolerated dose (monitoring hypotension or hyperkalaemia).
3. Add an SGLT2 inhibitor where indicated.
4. If the person has type 2 diabetes, consider adding a non-steroidal MRA to reduce CKD progression and CVD events.
5. If the person has type 2 diabetes, consider adding a GLP-1 RA, as early evidence suggests this may have benefits for kidney and cardiovascular outcomes.
To aid prescribing decisions, the new handbook introduces a ‘prescribe’, ‘reduce’ or ‘avoid’ classification system for medications in patients with CKD.
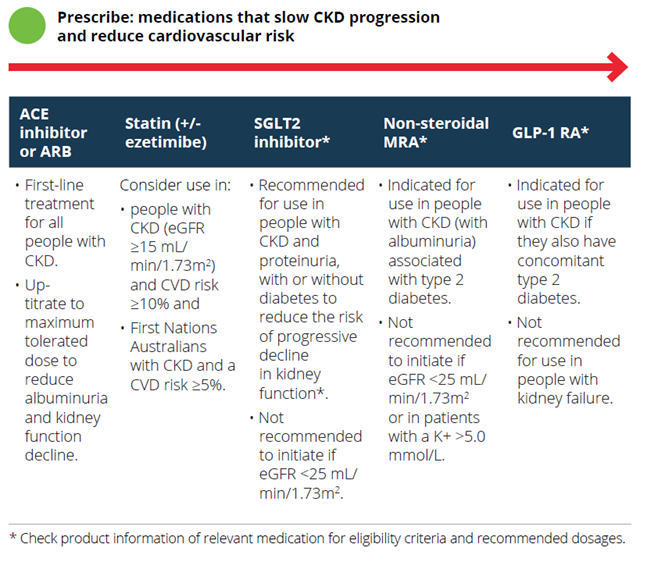
GPs can now prescribe two sodium-glucose cotransporter-2 (SGLT2) inhibitors for CKD management via the PBS, with research indicating these medications can lead to significant improvements in a range of outcomes.
The drugs now PBS-listed for CKD are:
Both these medications are streamlined authority.
A trial of empagliflozin found that compared to placebo, it reduced the risk of cardiovascular death and kidney disease progression in a range of patients with CKD, potentially delaying kidney replacement therapy by 2–27 years (depending on baseline eGFR).
Patients must meet specific clinical criteria to access these SLGT2 inhibitors via the PBS, making it essential to detect CKD as early as possible.
To be eligible, patients must have:
Patients can only be prescribed one SGLT2 inhibitor at a time and will need to stop taking it before starting dialysis treatment or having a kidney transplant.
“Expect a reversible drop in eGFR after patients start an SGLT2 inhibitor. This is greatest four weeks following initiation, after which the eGFR rebounds. Specific testing of eGFR for this purpose is not necessary,” Kidney Health Australia’s Breonny Robson explains.
SGLT2 inhibitors cause an osmotic diuresis, so consider reducing diuretics and/or antihypertensive medications if you initiate one.
While eGFR must be between 25-75 mL/min/1.73 m2 before initiating treatment, patients already taking an SGLT2 inhibitor whose eGFR drops below 25 mL/min/1.73m2 can stay on the medication until they can commence kidney replacement therapy — if it’s clinically appropriate, considering their other co-morbidities and any other relevant factors.
In addition to the SGLT2 inhibitors, finerenone (Kerendia) a non-steroidal MRA was also recently PBS-listed for use in people with CKD and type 2 diabetes, Ms Robson says.
“This provides yet another tool to treat CKD and can be used for people with diabetic kidney disease with an eGFR >25 mL/min/1.73m2 and a uACR >22.6mg/mmol. Patients must be stabilised for at least 4 weeks on either an ACE or ARB before initiation of finerenone, and it must be used in combination with an SGLT2 inhibitor. There are a few other prescribing criteria, and we recommend that GPs check the PBS listing.”
Two additional treatments have recently been approved for use to assist with CKD symptoms. This first is cation exchange polymer patiromer, which was PBS listed in September 2023 for use in hyperkalaemia, she says. The second is difelikefalin for CKD associated pruritis that was PBS listed on 1 May 2024 (note that this can only be used in a hospital-setting).
You usually need to cease or reduce the dose of medications excreted by the kidneys once GFR falls below 60 mL/min/1.73m2.
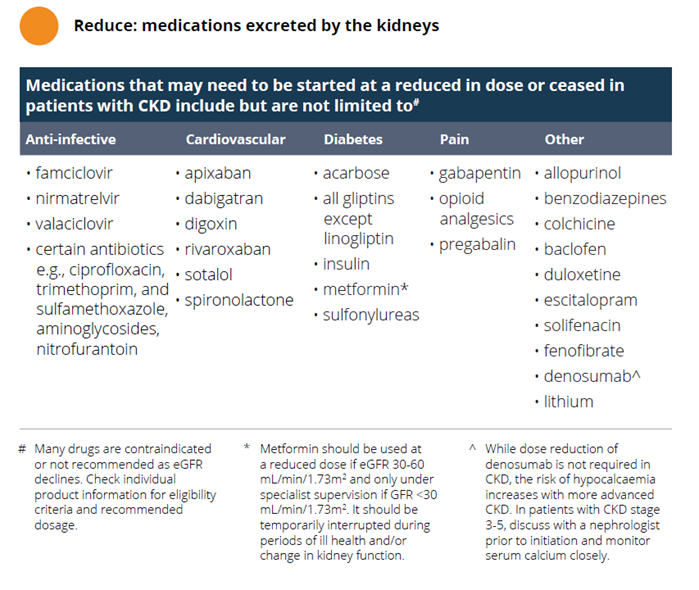
It’s particularly important to avoid nephrotoxic medications and ensure that patients know which ones to temporarily stop when they’re experiencing an acute illness.
These include lithium, aminoglycosides and NSAIDS/COX-2 inhibitors.
Be sure to avoid the ‘triple whammy’ – a dangerous combination of RAS blockade (ACE inhibitor or ARB), diuretic and NSAID or Cox-2 inhibitor (except low dose aspirin). It’s important to educate individuals taking an ACE inhibitor or ARB plus diuretic about appropriate pain relief medication.
It’s important to create a ‘sick day management plan’ that outlines which medications should be temporarily stopped during acute illnesses where people may become dehydrated from vomiting/diarrhoea or if they have a high temperature, as this can help prevent further damage to the kidneys, Ms Robson says.

Chronic Kidney Disease (CKD) Management in Primary Care (5th edition). Kidney Health Australia, Melbourne, 2024.
Images have been reprinted from the Handbook with permission from Kidney Health Australia.
Based on this educational activity, complete these learning modules to gain additional CPD.

STIs – Common and Tricky Cases

Role of Testosterone During Menopause – Evidence vs Hype

RSV Prevention in Infants and Pregnant Women

Vision and Driving Fitness: Key Insights for Health Practitioners



Yes
No
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
