Articles / 1 in 5 GPs fearful of violence from their mentally ill patients

In April, a man upset about the care his elderly mother had received in Canberra Hospital threatened to kill the doctor who had treated her, according to reports which allege he was agitated and erratic, with police concluding he had a mental disorder (despite his refusal to do a mental health assessment).
In an unrelated incident in January, a 34-year-old man was killed by police outside a medical centre south of Wollongong after pulling a gun on his doctor. He had been known to police due to “previous psychological medical episodes,” but had no prior history of violence.
These and other recent news events have drawn attention to the risks of inadequately treated serious mental illness, but just how often are GPs targeted?
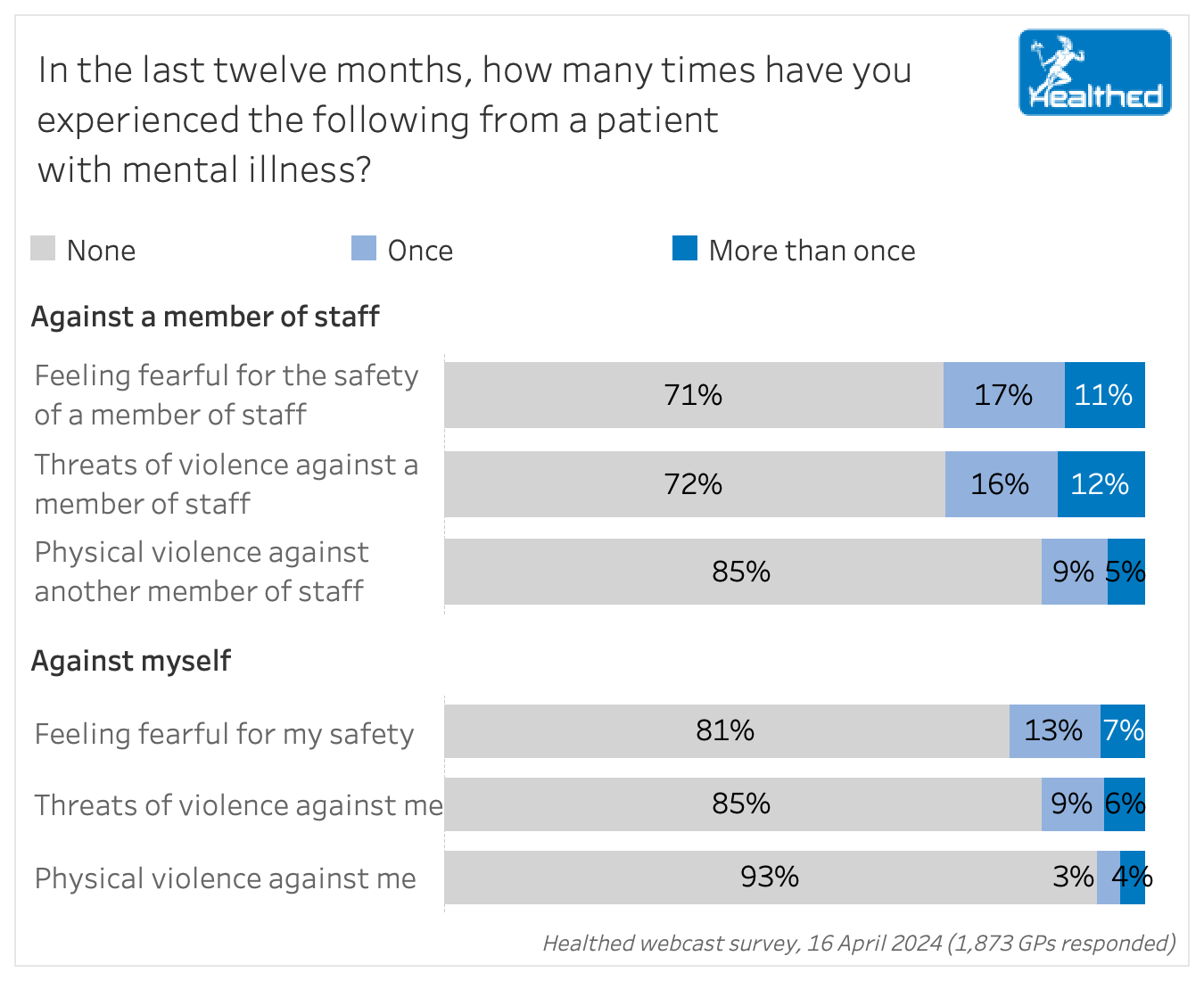
Healthed’s 16 April survey found that in the last 12 months alone, 28% of GPs had concerns for the safety of staff members at their clinic, and had colleagues who had been threatened by a patient who was mentally unwell.
Meanwhile 15% of surveyed doctors had personally received threats, and 7% had experienced direct physical violence when dealing with patients with a mental illness.
About three-quarters of GPs in Healthed’s follow-up survey on 30 April said there’s been no noticeable change in how often they or clinic staff have experienced physical violence or threats of violence from mentally ill patients in the last five years.
Fifteen percent said physical violence had increased in that period and 9% said it had decreased, while 18% said threats of violence had gone up, and 10% said they’d gone down.
The risk of violence is a reality in general practice, says Dr Ameeta Patel, chair of the board of Doctors’ Health NSW – an independent service that provides confidential phone-based support for doctors, medical students, dentists and vets.
While not new, this problem is compounded by systemic issues with mental health care, says Dr Mukesh Haikerwal AC – GP, Deputy Chair of the Australian General Practice Alliance and former AMA National President.
“We’re having many more people discharged to the community with very little follow up from state-based mental health services, and very little access to places to go or to escalate to if there are problems.”
“Basically, they’ve been cut loose from hospital, and we’ve been cut loose from any support.”
“So of course, if you ask the question, are you concerned about your safety in the practice? The answer is yes. Are you concerned about your safety because of mental illness? The answer is yes.”
Almost one in three survey respondents reported that staff had been threatened with violence, which Dr Haikerwal says is not surprising.
“Staff are subject to terrible abuse on the phone and face to face with veiled and actual verbal threats,” he says.
“Most of the time it does not become physically violent. And that’s probably because of the numbers of people around.”
“But if there’s a lack of security measures, including panic buttons, then not only will the staff feel more vulnerable, they’re also more likely to face assault.”
Threatening behaviours against staff have an adverse impact on the practice, he adds.
“It’s been hard to retain staff, it’s been hard to reassure people, because of that level of aggression that we do face.”
As has been widely noted, violence is often related to factors other than mental illness, and GPs may experience threats for several reasons.
One survey respondent said, “Most of the threatening behaviour from patients has nothing to do with their mental health problems. It’s usually related either to drug dependence or anti-vax beliefs.”
“Our major concern for safety is not from patients rather than from people in the neighbourhood – high rate of car theft and person assaults in our town,” said another.
Dr Haikerwal points out that some people are “just basically nasty.”
“And certainly since COVID, the level of nastiness has increased,” he says.
An analysis of more than 1000 free text responses in Healthed’s survey showed many practices are already taking steps to promote safety.
More than half of respondents (55%) had panic buttons in place for emergencies, and about one third proactively used de-escalation techniques, for example.
Maintaining continuity of care
“Keep regular contact with mental health patients a minimum of monthly. Don’t give repeats. Always show the patient respect. Know the patient.”
“Good long-term patient-doctor relationships reduces risk of threatening behaviour”
Prioritising good communication and respect
“Friendly communication and listening.”
“Communication strategies which include active listening and empathy to build rapport and diffuse potential threatening situations.”
Using de-escalation techniques
“Try to remain calm, and speak in a calm, clear and slow voice. Give the person some physical space, avoid confrontation.”
“Try to calm patient down and resolve the issue that triggers patients’ anxiety and distress.”
Minimising potential stressors
“Make sure that mentally ill patients get prompt appointments and don’t have to wait too long on arrival.”
Assessing and addressing risks
“Risk assessment of patients with known mental health issues, care plans to address potential risks, staff training to recognise signs of potential threat, review of safety procedures.”
Setting boundaries for acceptable behaviour
“We implemented rules and regulations about these behaviours. we put it clearly on the voice message and advertised it in the waiting area. Moreover, we fired the misbehaving patients.”
Practical training and protocols
“Specific training on how to diffuse difficult situations, how to physically protect oneself.”
“The receptionist will inform us if the patient is agitated, so we settle them in a private room and attend with a chaperone.”
“Make sure the way to the door has no obstacles (e.g. the table or couch).”
“Panic buttons installed in each consulting room.”
Dr Patel from Doctor’s Health NSW recommends strategies like the ones cited above, adding that it’s important to abide by legal and ethical requirements, especially regarding confidentiality and safety.
“Your medical indemnity provider is available to assist you to navigate these requirements when dealing with a difficult patient,” she says. “They can also provide advice on how to ‘break up’ with a difficult patient when necessary.”
Dr Haikerwal notes GPs are generally very aware of their responsibilities to staff and patients, including those with mental health issues.
“Obviously, you don’t want to discriminate against one sort of person or other, because of their illness,” he says.
There is a need to balance patient rights and staff safety, however.
“Security has to come first,” Dr Haikerwal says. “From a governance point of view, from an owner point of view, from a work safe point of view, we strive to minimise exposure of our staff to these dangers.”
Harking back to pandemic days when patient agitation was at a peak, he says security patrols in the building where his practice is located helped mitigate verbal and physical abuse.
Access to CB radios was also a big help.
“It’s a very useful thing to summon help quickly without having to dial a number and hope somebody will pick up at the other end.”
If you’ve experienced violence or threats, Dr Patel recommends seeking support from colleagues and organising a check-up with your GP or psychologist.
The RACGP has resources for preventing and managing patient aggression and violence.
Doctors’ Health NSW operates a 24/7 confidential phoneline staffed by experienced, non-judgemental doctors. Call 02 9437 6552.

RSV Prevention in Infants and Pregnant Women

STIs – Common and Tricky Cases

Role of Testosterone During Menopause - Evidence vs Hype

Vision and Driving Fitness: Key Insights for Health Practitioners
Yes
No
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
