Articles / Triple incentive a win for bulk billing, or smoke and mirrors?

In a recent media blitz, the Government sang the praises of the tripled bulk billing incentive from the rooftops. In a five-month period, the national bulk billing rate rose 2.1% ─ reaching 77.7% in March — and stopping a decade-long downward slide.
Yet, Healthed’s most recent survey of more than 1900 GPs found that the policy had marginal impact in real-world terms.
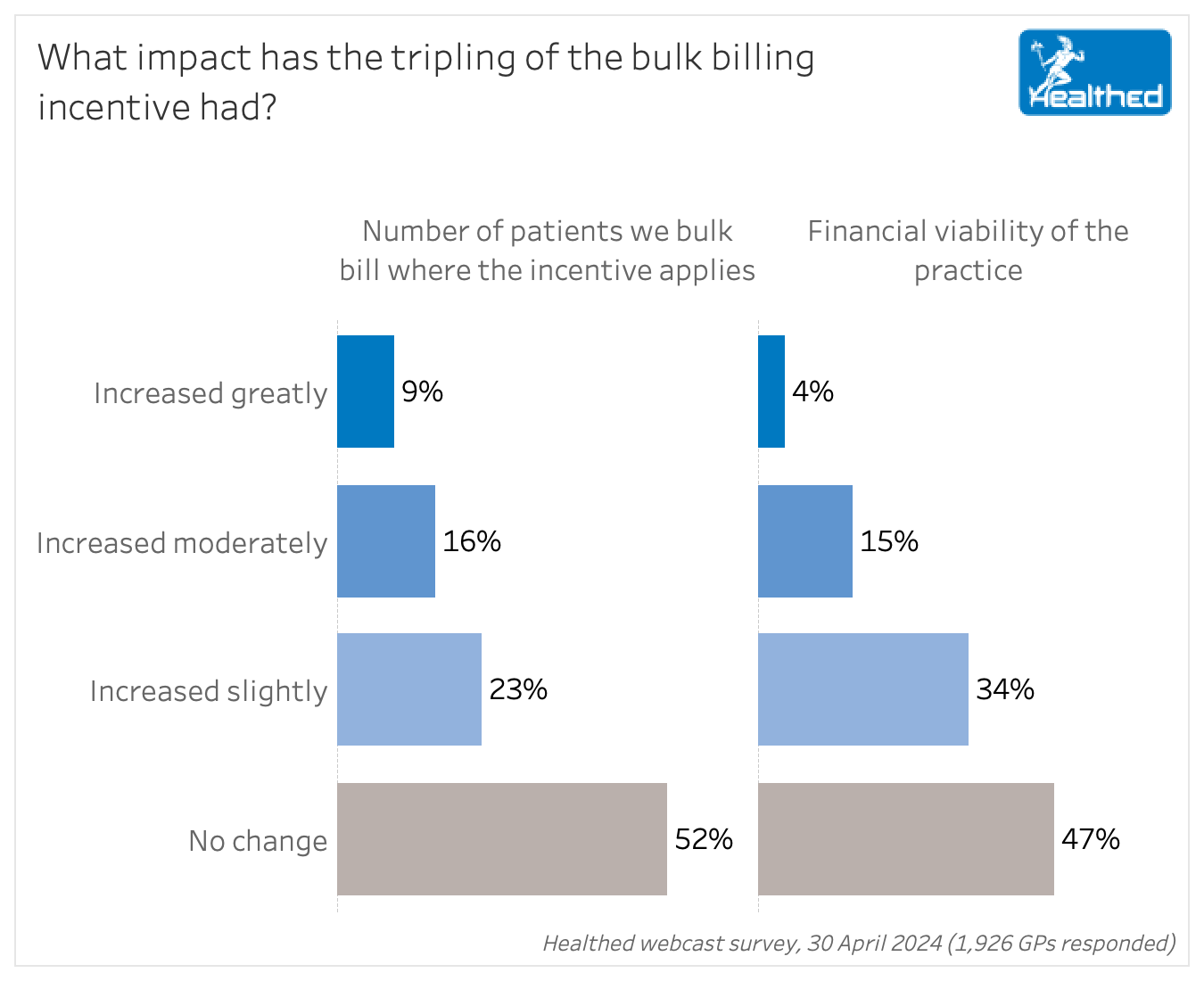
Perth GP and Clinical Associate Professor Pradeep Jayasuriya says the survey findings suggest that “the tripling of the incentive has had a marginal impact on patient access to care and the financial health of GPs.”
“But, unfortunately, it’s far from enough, and certainly not the game changer that it was trumpeted to be. And I think that underscores the fact that the plight of general practice is a lot more complex than a small financial change,” Associate Professor Jayasuriya continued.
So has the initiative halted or reversed the trend away from bulk billing?
“I think the answer is it may have halted it, but it hasn’t reversed it to any substantial extent,” Associate Professor Jayasuriya said.
Health economist Professor Stephen Duckett, of the School of Population and Global Health and in the Department of General Practice and Primary Care at the University of Melbourne confirms that.
“The reduction that was occurring in bulk billing has plateaued,” Professor Duckett says.
“There’s been a tiny, tiny uptick in the proportion of attendances bulk billed, but there’s been no further decline. So the government, I think, can rightly claim to have arrested the decline.”
What remains unclear is how long the halt can last as the inevitable economic factors and cost of living continue to bite.
There may be multiple factors at play.
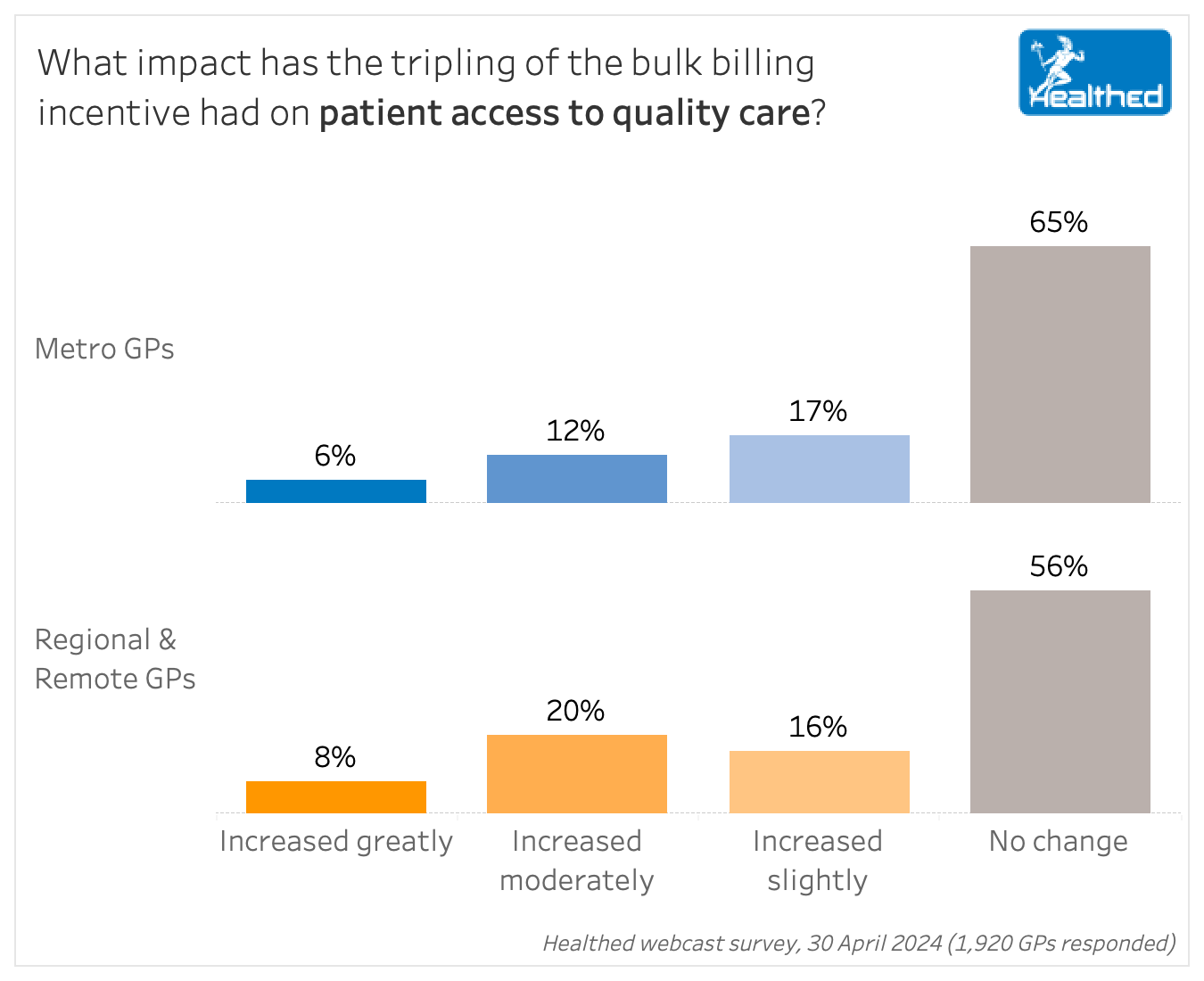
Professor Duckett says the most important predictor of the impact of the tripled incentive is where you practice.
Greater impact in rural and remote Australia
While the tripled incentive has had minimal impact for most of the country, there’s been more improvement in rural and remote Australia, according to Professor Duckett.
“So the tripling of the bulk billing incentive was really, really, really good for rural and remote areas. It essentially covered the gap, so it was really significant…That was the highest tier,” he says.
In contrast, the lowest tier was in metropolitan Australia, where the tripled incentive only accounted for about one-third of the gap being charged.
“There was no impact in metro because the average out of pocket cost was much, much higher,” Professor Duckett says.
Given that about three quarters of survey respondents and GPs nationally live in cities, he wouldn’t expect to see a huge change overall.
Healthed’s survey found regional and remote GPs were more likely to increase the number of patients they bulk billed, report improved practice viability, and say the incentive had improved their patients’ access to quality care, compared to their urban colleagues.
How the billing rate is calculated
Another factor that contributes to the discrepancy between the bulk billing rate reported by the government, and GPs and patients on the ground experience, is the way it’s calculated, Associate Professor Jayasuriya points out.
People often intuitively think the reported rates refer to how many people are bulk billed, but in fact, they refer to proportion of GP visits that are bulk billed.
This leads to a more impressive number. An August 2023 report from the Department of Health and Aged Care notes that the proportion of patients who are bulk billed 100% of the time tends to be lower than the bulk billing rate. This is because many GPs will bulk bill some, but not all, consultations with the same patient. Moreover, GPs may be more likely to bulk bill for more frequent and shorter consultations, Associate Professor Jayasuriya adds.
The report showed that 51.7% of patients were always bulk billed, 25.6% were usually bulk billed, 12.2% were sometimes bulk billed and 10.5% were never bulk billed. (And one in 14 people delayed or did not visit a GP last year due to cost, ABS data shows).
The fickle nature of politics
GPs may also be reluctant to change their billing practices because there is no guarantee that the policy will be permanent, Associate Professor Jayasuriya speculates.
“To change your billing practices requires a significant change in practice policy and it means changing back again if the incentive disappears,” he says
“I still remember the day when the rebate rises were frozen literally at the stroke of a pen overnight. You are at the whim of government. And I think many GPs still remember that and there’s a sour taste in their mouth.”
Too simplistic of a solution
In Associate Professor Jayasuriya’s view, the survey numbers suggest that overall, the tripled incentive hasn’t made any inroads into the health of GP practices.
“It was always naive to think that one initiative like this in primary care was going to fix the problem, because the problems are multifaceted and more complex than simply one of increasing a few dollars to a portion of the population. The issues are much more entrenched and complex.”

RSV Prevention in Infants and Pregnant Women

STIs – Common and Tricky Cases

Role of Testosterone During Menopause - Evidence vs Hype

Vision and Driving Fitness: Key Insights for Health Practitioners
Yes
No
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
