Articles / Older GPs’ fitness to practice? Poll results are in

Younger GPs overwhelmingly favour assessing fitness to practice for late-career doctors, but their older peers are less convinced, according to a snap poll of over 500 GPs who attended Healthed’s Women’s & Children’s Health Update in Sydney on 10 August.
Earlier this month AHPRA and the Medical Board opened consultation on three options aimed at “keeping late career doctors in safe practice,” explaining that doctors aged over 70 are 81% more likely to be the subject of a notification for any reason (not just impairment) than those aged under 70.
More than 70% of GP respondents aged 25-44 agreed with the Board’s proposal to introduce general health checks with a GP for doctors aged 70 and older, “to support early detection of concerns with the opportunity for management before the public is at risk.”
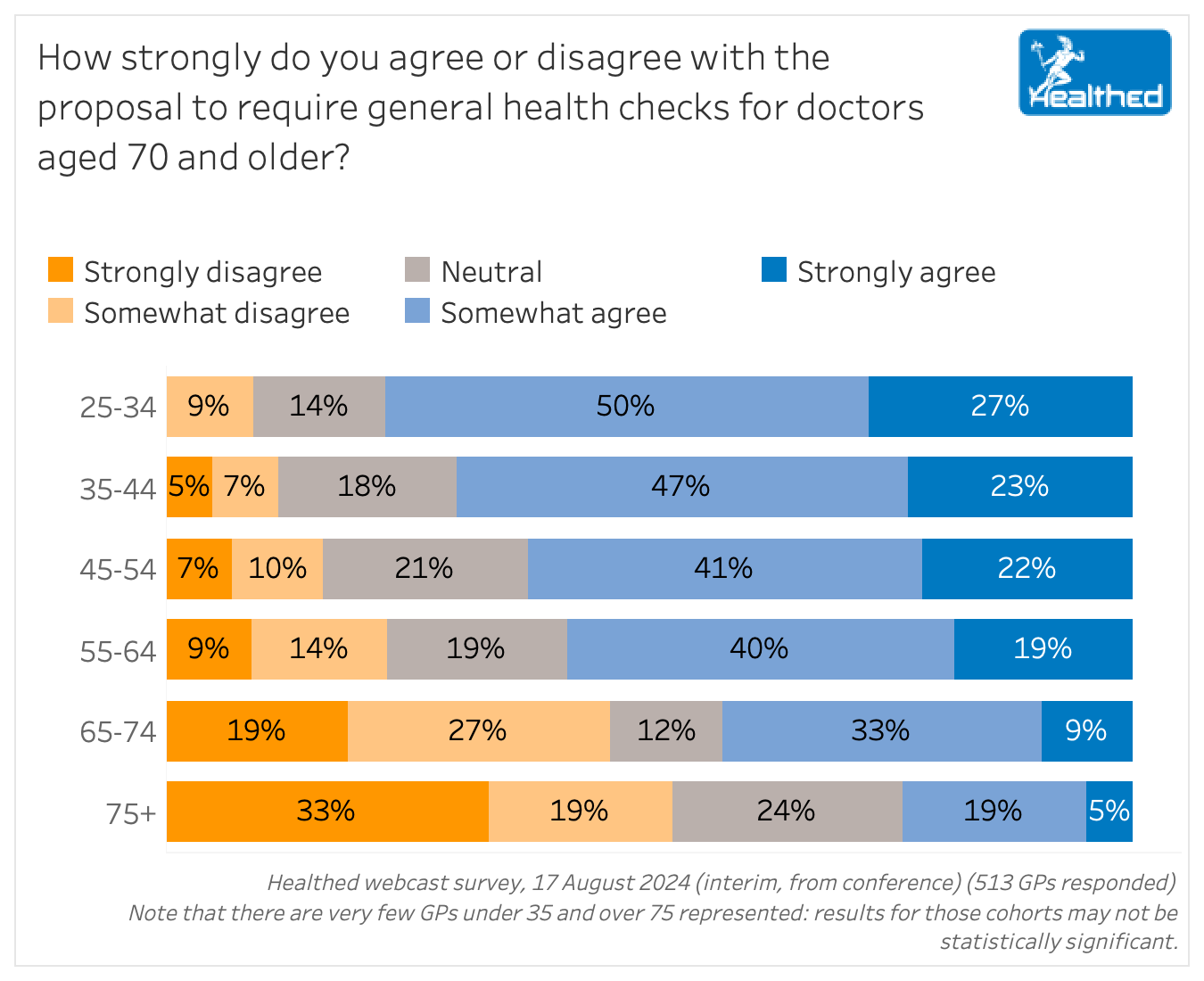
Across all age groups, 59% of GPs were generally supportive, 18% were neutral and 24% were generally opposed to that specific proposal.
But there was a clear correlation between the age of survey respondents and their views on regulatory changes, with support dwindling with each decade.
While the Board is seeking feedback on three options, including extensive assessments with specialist occupational physicians, as well as keeping the status quo and doing nothing extra, they have stated overtly that they favour the mandatory general health checks by a GP or other doctor.
The Board said this option would be “best for patient safety and for keeping doctors in control of their careers as they age.” From age 70, doctors would have to undergo general health checks with their GP or another doctor every three years, and yearly from 80 years of age, they explained.
When Healthed asked GPs about the three options more broadly, a clear majority (60%) supported that approach, while younger doctors were slightly more open to requiring a detailed assessment from a specialist occupational physician, and older GPs had a clear preference for maintaining the status quo.
Again, the same age-related trend was present, with the youngest GPs most likely to support interventions, and the oldest GPs least likely to.
Professor Karen Price, immediate past president of the RACGP, GP and researcher, said that while it’s important to encourage doctors to have regular health checks given their propensity to neglect self-care, forcing them to do it is not the answer.
“In my research and experience it seems the nudges to perform self-care are more likely to be enacted when a well-known peer nudges you firmly, than an unknown assailant from the health department,” Professor Price said.
She had some words of advice for the youngest cohort in the survey: “all I can say is that time goes quickly and being older comes quicker than cognitive decline. Good luck with the galloping passing of time.”
However, she noted that most doctors steered away from the most punitive option.
“It seems interesting and encouraging within these results, however, that the punitive mind set of enforcing examinations is in the minority,” Professor Price said. “As I would expect from my educated colleagues, a more thoughtful approach that has less imminent threat was preferable if there was to be anything at all.”
More information on the proposals and consultation process is available on AHPRA’s website here.

RSV Prevention in Infants and Pregnant Women

STIs – Common and Tricky Cases

Role of Testosterone During Menopause - Evidence vs Hype

Vision and Driving Fitness: Key Insights for Health Practitioners
Yes
No
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
