Articles / Reduce 10-year rural requirement for IMGs – GP poll

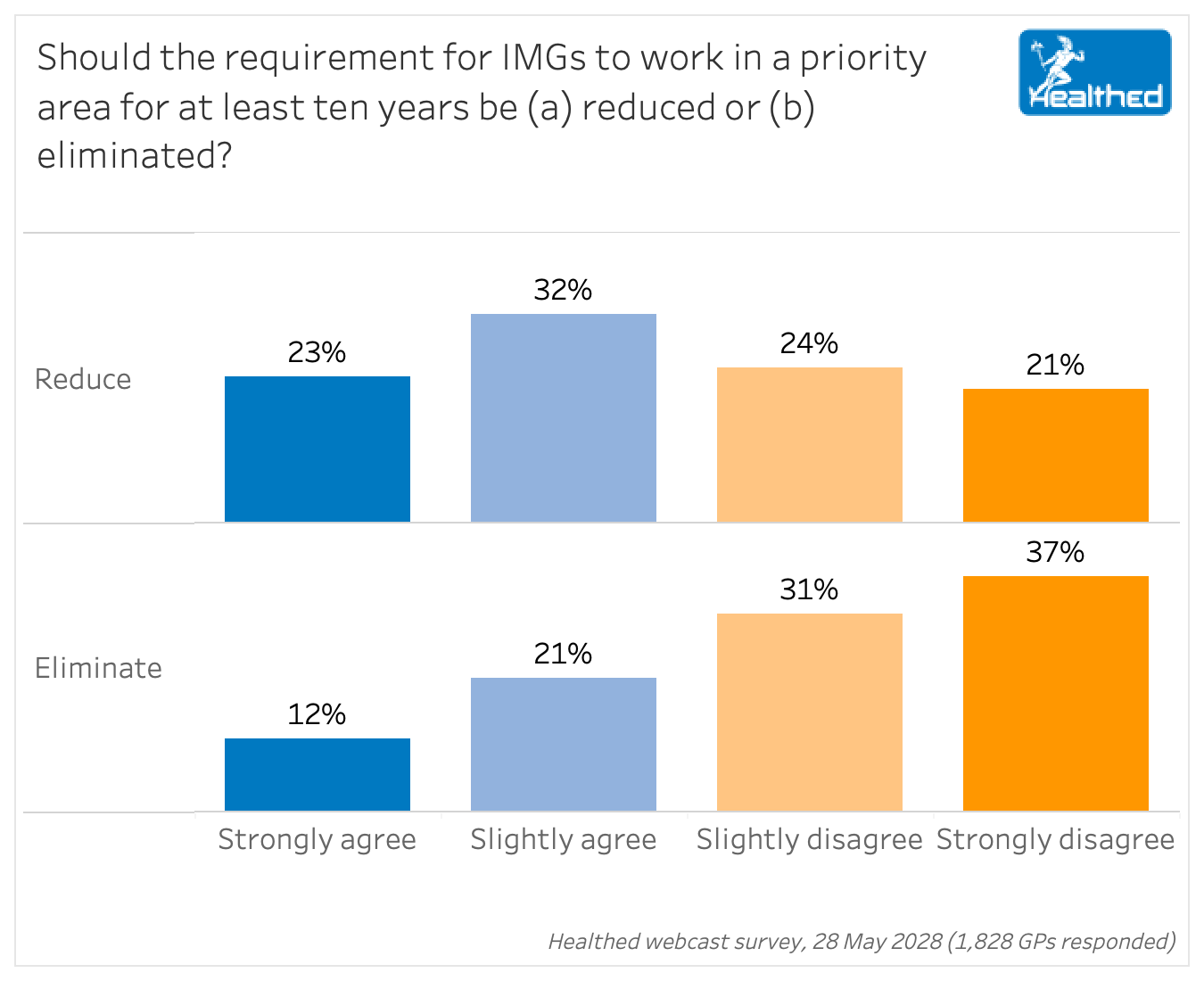
Fifty-five percent of GPs think the length of time international medical graduates (IMGs) are required to work in a priority area should be reduced — but just one out of three think the requirement should be scrapped entirely, a national Healthed survey of 1800 GPs found.
Despite calls from the RACGP to remove geographic practice restrictions for IMGs who’ve completed fellowship training, the policy was not addressed in the independent Kruk report.
The RACGP has never supported the moratorium. In their submission to the review, they argued that a class exemption to the 10-year moratorium would make Australia more attractive for doctors who trained overseas, particularly those whose spouses have been employed by large hospitals in metropolitan areas.
While 68% of GPs responding to Healthed’s survey did not support eliminating the policy, many felt a decade was “too long.”
“There is already a workforce shortage in the rural setting, thus I think IMGs just have to work there if they want to migrate to Australia,” one GP told Healthed. “However, I believe they should not be required to be out there for 10 years. The government just has to find ways to attract Aussie doctors to go back to rural to work.”
“At least the duration should be reduced following permanent residency or citizenship,” another GP commented.
The existing policy includes measures IMGs can take to reduce the length of the moratorium, known as scaling. Working in a very remote area, for example, can reduce the time by half.
But many GPs have raised concerns about lack of support for IMGs working in isolated areas.
“Having worked in a regional area myself more than 13 years, there is lack of resources and mentor support in regional and rural areas. IMGs are left to fend for themselves and funding is under-utilised or incorrectly distributed,” one respondent wrote.
RACGP President Dr Nicole Higgins agreed this is a key issue.
“Putting the most vulnerable doctors in the most vulnerable communities without support can be a recipe for disaster for both the doctor and the patients,” Dr Higgins told Healthed.
“These are doctors who have to learn Medicare and our pharmacy system. They have to understand Aboriginal and Torres Strait Islander culture and also what it’s like to work in a rural and regional area, as many of these doctors have come from urban places and very different cultures.”
GPs who received their qualifications overseas were more likely to oppose the 10-year requirement for IMGs to work in a rural area – with 41% saying it should be eliminated, compared with 24% of GPs with Australian qualifications. Likewise, GPs who trained overseas were more likely to strongly agree that the length of time required should be reduced.
However other GPs worried that reducing the time IMGs must work in priority areas would exacerbate workforce shortages.
“We already don’t have enough doctors in rural areas and if the 10-year moratorium is eliminated we won’t have GPs in rural communities at all,” one GP said.
Dr Higgins said doctors should be supported to work in priority areas, not directed where they must work on entering the country.
“This means things such as childcare, schooling, connecting people with community, ensuring that they have access to their own culture and faith within communities where they will work,” she said.
“That’s what makes them more likely to stay in a community versus being forced.”
She cites the example of 177 new GPs in training “that have been placed in difficult areas that haven’t had GPs, some for a significant period of time.”
“Those doctors, if they’re supported, we’ve found that two-thirds are actually staying beyond their placement time.”
Some GPs commented that the policy should extend to all GPs, not just IMGs.
“All medical graduates (IMGs and Australian) should equally serve areas of need. Don’t discriminate,” one GP commented to Healthed.
“IMGs who would like to work in priority areas will remain in those areas. There is no need to coerce anyone. If there is a mandatory period of community service by medical practitioners, it should be applied to all medical practitioners in Australia,” another GP said.
Dr Higgins says while she’d love every doctor to receive rural or remote experience, achieving this would necessitate some changes.
“Our average age of a registrar is now 34,” she explains, “which is the peak time when people are raising families, paying off mortgages, and already embedded in their communities.”
“If we’re going to get doctors to work in rural and regional Australia, we actually need to start earlier in the pipeline, and that means recruiting medical students from rural and regional Australia, allowing them to train where they live and providing the incentives and supports for our medical students to have rural and regional exposure.”

RSV Prevention in Infants and Pregnant Women

STIs – Common and Tricky Cases

Role of Testosterone During Menopause - Evidence vs Hype

Vision and Driving Fitness: Key Insights for Health Practitioners

Yes
No
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
