Articles / Pharmacy prescribing is now nation-wide: how will it impact your clinic?

Pharmacists across the country can now diagnose and manage uncomplicated urinary tract infections (UTIs), with the Northern Territory becoming the last state or territory to expand pharmacists’ scope to do this last week.
More than 6000 community pharmacies around Australia have the opportunity to provide prescriptions for everyday health conditions, the Pharmacy Guild said.
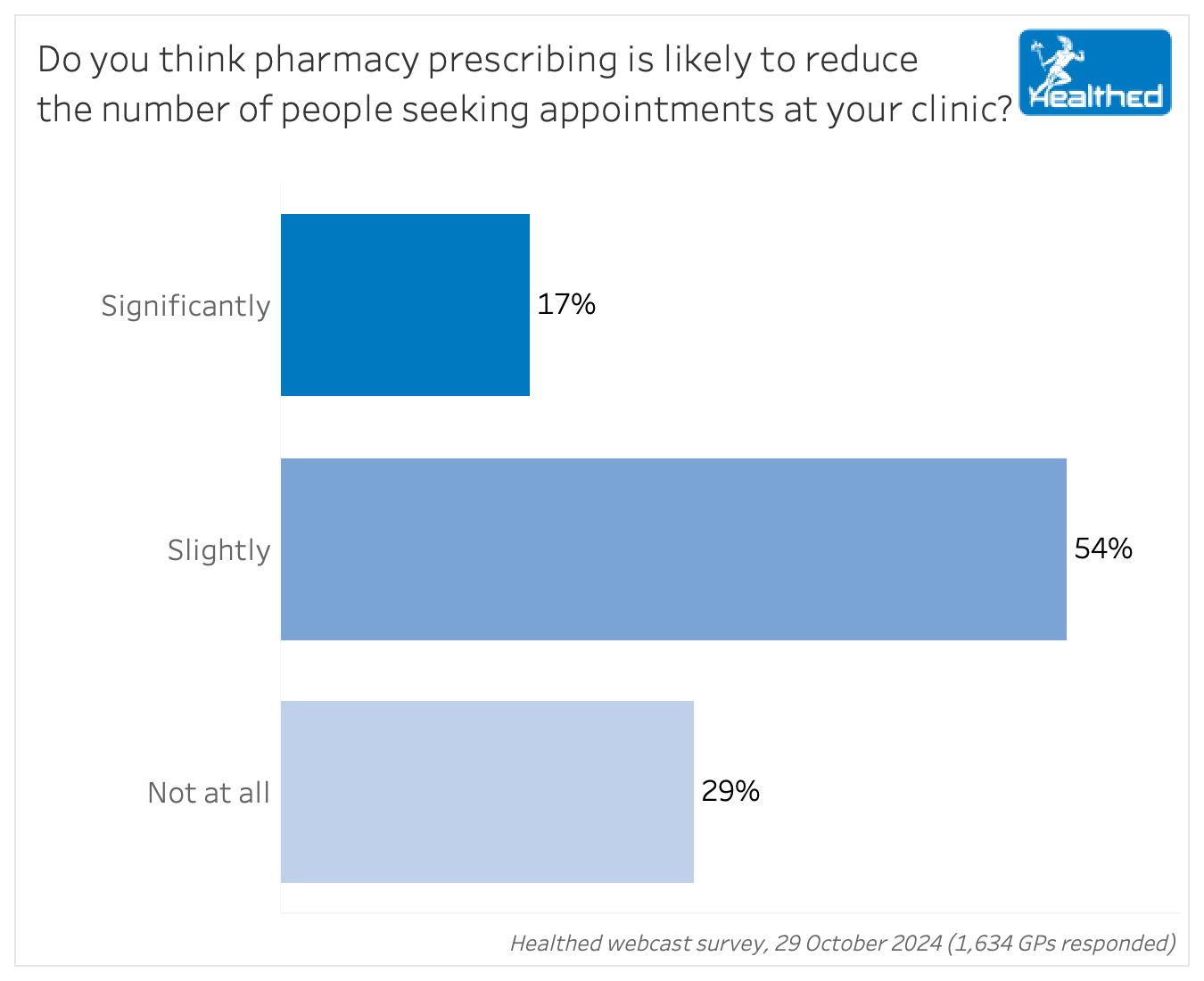
With pharmacy prescribing now national, we asked GPs about the likely impact on the number of patients seeking appointments at their clinic.
Overall, 71% of GPs think pharmacy prescribing will lead to fewer patients seeking appointments — of those, 54% think it’s likely to be a slight reduction, while 17% expect a significant reduction.
The remaining 29% say pharmacy prescribing is not likely to impact this metric, our national survey of more than 1600 GPs found.
Some GPs considered fewer patients booking in to be a positive, saying they were just too busy to see everyone in a timely manner, for example. Others said impact on patient numbers would be minimal, as patients continue to come in for a second opinion or to discuss their situation further. Still others felt that reduced appointments could have worrying unintended consequences.
“This will have a negative effect on patient care as the visits for script renewal allow us GPs to discuss preventative care and other issues such as psychological health,” one GP who expected a significant reduction in visits said.
“Pharmacy prescribing causes me so much trouble, as the patients cannot tell me what they were given and tried already, and the situation is so much worse when it comes to me.” – surveyed GP
“Pharmacists are already overusing the inappropriate antibiotics and not testing appropriately first. Patients present more unwell to GPs, and we have no MSU (for example) to refer to when the antibiotics given by the pharmacist have not worked. I am extremely concerned about increasing unnecessary antibiotic use, antibiotic resistance, and increased sepsis in incorrectly treated patients. Also STDs being missed. Also lack of patient confidentiality in pharmacies,” another GP said.
“Already we see that there are less patients making appointments. Usually patients will go to the pharmacist or allied health for their problem for three to four weeks before presenting. Conditions are more progressed than they need to be or a lot of mixed treatment given, and not improved. As patients move to pharmacists for simpler health care, GPs will get more chronic cases and patients with more issues,” another GP commented.
The Healthed survey results coincide with the final report of the Scope of Practice Review released Tuesday, which has been sharply criticised by the RACGP.
“This is a report, not a plan, but its recommendations will raid Medicare and set us up for a two-tiered health system where those who can afford to see a GP will, and those who can’t, don’t,” RACGP president Dr Nicole Higgins said.
She took aim at the recommendation to allow allied health professionals and others such as nurses and pharmacists direct referral pathways to specialists that would bypass GPs, saying it won’t improve efficiency or cost effectiveness for patients.
For example, the report recommends that chiropractors and osteopaths could refer directly to orthopaedic surgeons, diabetes educators could refer to endocrinologists and podiatrists to vascular surgeons – to name a few of the specific examples listed.
Dr Higgins said this would remove coordination of care from a GP who has their broader context and history front of mind.
“Dropping that coordination will lead to a free for all, without a GP’s oversight to ensure care is necessary and in a patient’s interest, and not doctors and other health professionals duplicating each other’s work,” she said.
Meanwhile the AMA is urging the government to respond cautiously to the report, which it said seemed to suggest adopting an “an NHS-style approach that has doomed primary care in the UK.”
“The federal government has acknowledged there is a GP workforce shortage, but it must resist implementing band-aid solutions that will only make the situation worse, as seen in the UK,” AMA President Dr Danielle McMullen said.
“Turning this shortage around requires comprehensive reform, involving greater investment in support measures for Australia’s highly valued GPs,” she said.
“My concern is just the poor practice it engenders. Take UTIs: is anyone going to examine a patient at a pharmacy counter? I am sick of people being asked personal questions to elicit confidential information next to other patients; most chemists don’t have examination rooms to assess and prescribe privately. And in central Australia there is a severe problem of antibiotic resistance to common agents to treat UTIs; not all dysuria is a UTI. Will appropriate pathology tests be collected? How much STI or PID will be (mis)treated as a UTI in the local chemists?”
“This will free up some time to deal with patients presenting with chronic and acute conditions,
but it will increase the likelihood of inappropriate prescribing and patients not having adequate follow up of their medical conditions (e.g. diabetes, asthma, heart failure, hypertension etc).”
“I’m more concerned about the potential for patient harm through missed or inappropriate diagnoses.”
“It’s about having lost the opportunity to provide the overall holistic patient care by taking into consideration other crucial factors about patients’ presentation and their underlying co-morbidities.”
“While this appears like a quick fix, certain diagnoses may potentially be missed and if there is inadequate communication between treating team and may lead to long-term adverse outcomes for patients – and in most cases the poor GP getting all the blame.”
“I am concerned about the increased likelihood of delayed patient presentation.”
“We will see more patients with partially or inappropriately treated conditions requiring more complex diagnosis to sort out what the initial situation was.”

RSV Prevention in Infants and Pregnant Women

STIs – Common and Tricky Cases

Role of Testosterone During Menopause - Evidence vs Hype

Vision and Driving Fitness: Key Insights for Health Practitioners
Yes
No
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
