Articles / GPs support more health professionals referring, IF…

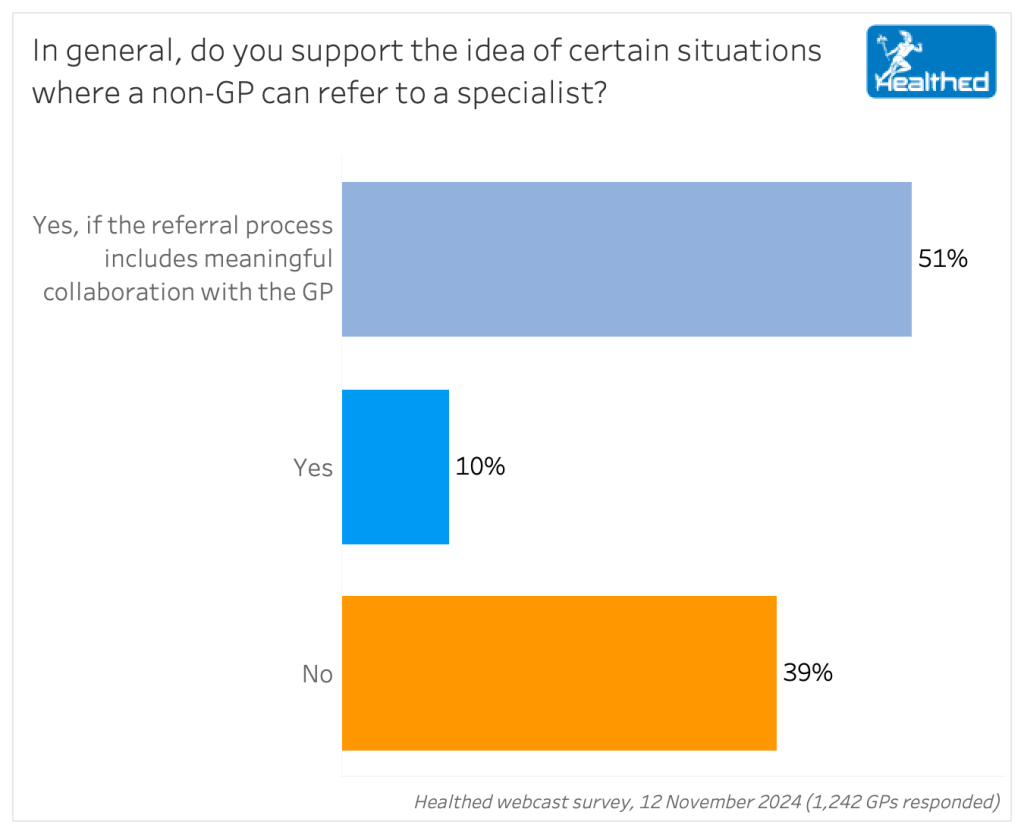
While the RACGP has expressed blanket opposition to allowing non-GP health professionals to refer to specialists, only 39% of GPs at the coalface share this position, a national Healthed survey of 1242 doctors working in primary care has found.
Although just 10% of GPs unequivocally support the recommendation that was put forward in the final Scope of Practice Review report earlier this month, a further 51% would support expanding other health professionals referring rights under the condition that the process specifically involves a collaborative approach with a GP.
Several survey respondents explained that GPs would need to be notified of the referral contemporaneously and cc-ed in on all correspondence – both from the health professional who makes the referral, and from the specialist – also noting that up-to-date reports and treatment information from the specialist, including any medications initiated, would be crucial.
“GP should be copied in on all correspondence to be kept in the loop.” – surveyed GP
There were also significant differences in support for some health professionals referring compared to others when we asked GPs to weigh in on the specific examples recommended in the report.
Notably, eight out of 10 GPs oppose allowing chiropractors or osteopaths to refer to orthopaedic surgeons. Similarly, nearly three-quarters of GPs did not support allowing dietitians to refer to gastroenterologists. Around two-thirds of GPs disagreed with allowing midwives or nurse practitioners to refer to psychiatrists, and the majority also did not support nurse practitioners referring to geriatricians, urologists or gynaecologists.
However, on the flip side, around eight out of 10 GPs support remote area nurses referring to medical specialists, and seven out of 10 agree that midwives should be able to directly refer to an obstetric physician or anaesthetist. Likewise, 61% support audiologists and speech pathologists referring to ENT surgeons, and 61% say psychologists should be able to refer to psychiatrists.
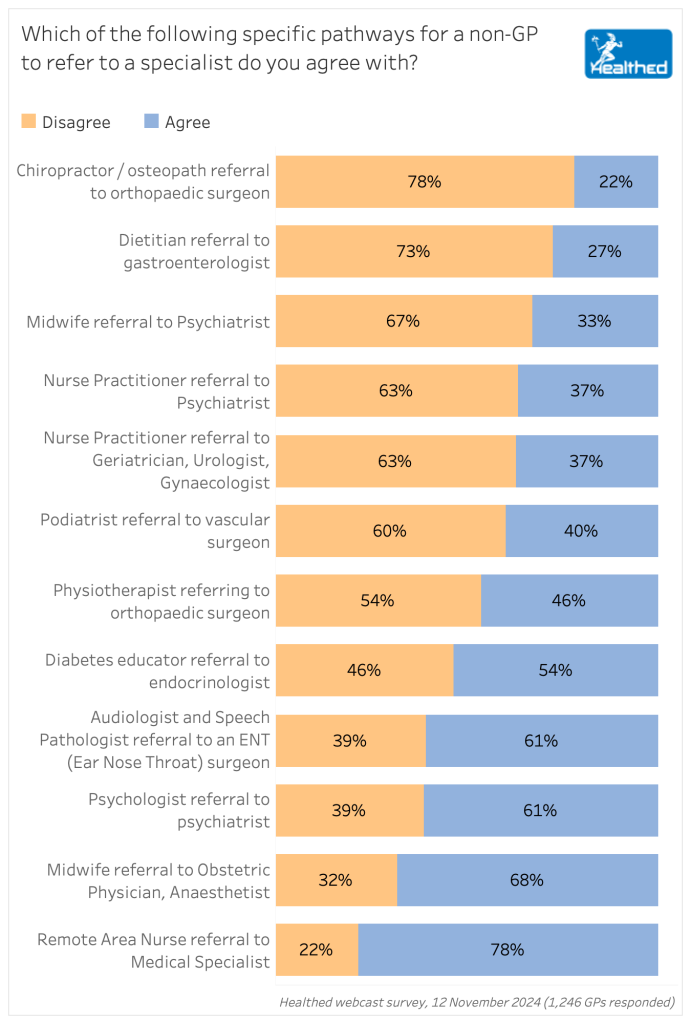
More than one quarter of over 100 GPs who provided additional comments in the survey pointed out that optometrists already routinely refer patients directly to ophthalmologists – with most citing this as an example of where it works well, though some said they do feel out of the loop sometimes as a result.
“I agree with referrals from optometrists to ophthalmologists as they will often pick up concerns regarding vision. Unfortunately, we do not always receive the information from the ophthalmologist,” one GP commented.
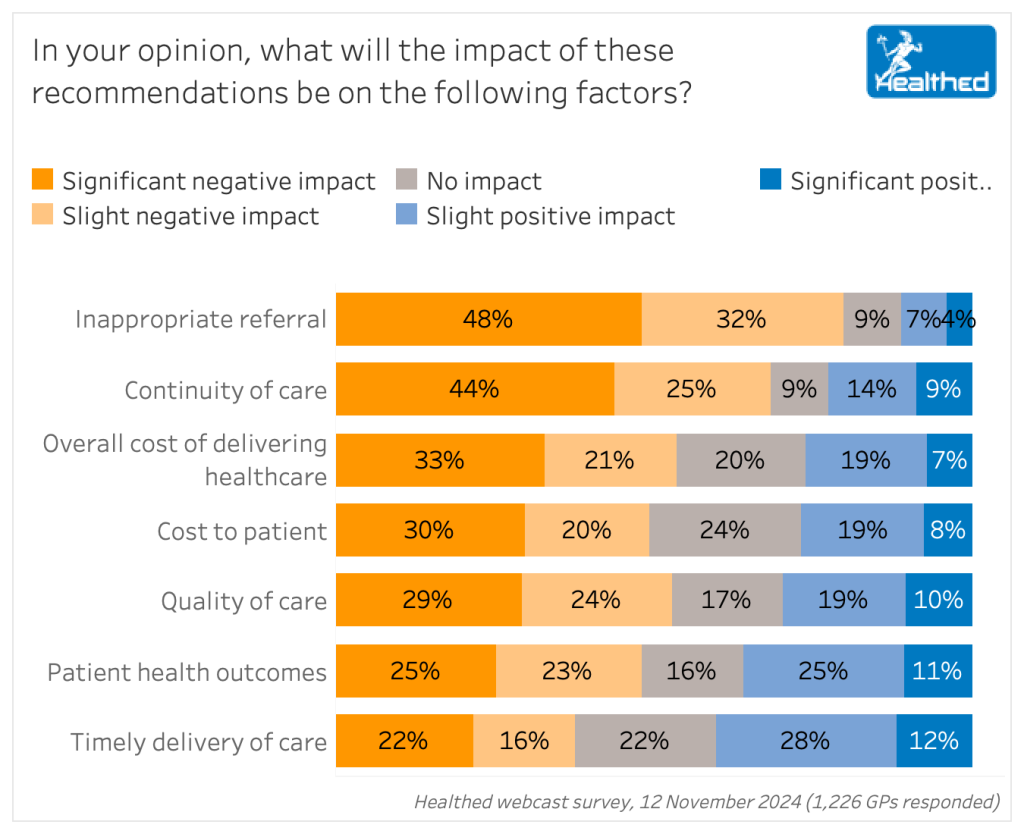
GPs are divided in their predictions regarding the timely delivery of care, with 41% expecting a positive impact, 35% expecting a negative impact and 23% predicting no impact.
“The hold up in seeing specialists is NOT due to the lack of referrers to specialists, it is due to the lack of specialists, especially in the public system. I cannot see that non-GP referrals would improve this, if anything, it might make the situation much worse due to potential inappropriate referrals clogging the system further,” one GP said.
“We have to be careful as to not overburden the health system with too many unnecessary specialist referrals and lengthier waiting times.”
Despite most GPs being open to other health professionals referring as long as there’s effective collaboration,81% think it will have a negative impact on inappropriate rereferrals—with nearly half predicting a significant negative impact. And 69% say it will have negative impact on continuity of care.
“In some situations it could be helpful, but it is likely to lead to cost blow-outs and fragmentation of care,” said one GP.
“This will likely involve much more triaging by specialists – expense to patients but may be helpful if it facilitates patient care. Governments have no idea how much we save the health system by prudent referrals for care,” another GP commented.
“Affects whole-person-centred care if their care is fragmented. It will not cut down wait time to see non-GP specialists – this process may even increase wait times if more people are being referred.”
Given how nuanced GPs perspectives are, it’s worth asking whether the peak bodies might be damaging their leverage by campaigning against non-GP referrals in such all or nothing terms. Perhaps if the RACGP lobbied in a more strategic and nuanced way here, they’d have more negotiating power for more pressing issues later…time will tell.
• Holistic care is crucial
“You don’t know what you don’t know. GPs have the privilege of long-term and comprehensive information about patients, have a broad training and can assess systemically what pathology may be happening. We try to maintain a history of investigations and can assess for changes and direct to appropriate specialist involvement. I have experienced complete incompetence by allied health workers misdiagnosis of presentations.”
“The GP is better placed to consider a more holistic approach and a referral that ideally provides useful information, such as up to date medicines list, social factors that may impact management, comorbidities, fitness for surgery etc.”
“They do not have access to the full situation – past history, meds, path, investigation, past specialist assessments. Equally applies to remote telemedicine services who have no longer term relationship with the patient.”
• Continuity of care
“If a non-GP allowed to do a referral the follow up process will not be easy and it will be a poorly coordinated care.”
“The care becomes too fragmented without a central place where there is summary of the issues. Relevant Past Medical history ends up being omitted from the GP’s notes.’
“If this goes ahead I can predict, more fragmented care, and the inability to see specialists as these non GPs will be referring LOTS of people.”
• Inappropriate referrals
“The main risk is that the allied health provider (as with anyone working in a specific area) doesn’t see the whole picture as a GP would, and therefore funnels referrals to doctors in inappropriate fields.”
“The negatives outweigh any perceived positives. It will lead to fragmentation of care with subsequent negative health outcomes and potential overloading of secondary care by inappropriate and unnecessary referrals.”
• Impact on costs
“Costs to patients will increase if referral is not appropriate. Non-GP referrals will also bounce back when declined or full books etc and the patient will end up at the GP office again after wasting time and money.”
• Effective collaboration is the crux
“A lot depends on the ability of the different practitioners to communicate meaningfully and ensure appropriate handover between professionals to maintain continuity of care and mutual understanding between all parties.”
“I am supportive of non-GP referrals to specialists within that person’s expertise provided they actually know what I as the person’s GP am also capable of doing without needing a specialist or while waiting for a specialist appointment. But MUST include the GP in the referral as often people go to ophthalmologists direct from optometrist & we have no idea what’s going on.”
• Scope needs to be carefully limited
“Only certain specific conditions. This should not be a carte blanche for mass referrals from allied health professionals. Those allied health professionals should undergo assessment/education with regards to the reason for referral and always should be in conjunction with a GP.”
“It would be interesting and possibly helpful if pharmacists can refer to specialists in the field of medication reactions, that they may have more understanding of.”
“While some of the above-mentioned professionals would no doubt have the expertise and insight to refer to a specialist, I still feel that it remains in the patient’s best interest for there to be a single gatekeeper who retains oversight of where the patient is being seen. I make an exception of rural nurses as they often work where there are no GPs to fulfill that role. I would be happy for referrals to be done in emergency situations with the proviso that the GP needs to be copied into the specialist referral.”
• Too many potential negatives
“This will cause fragmentation, increased specialist costs, repeated assessments when presenting to dual practitioners and cut GPs out as coordinators of care. There will be loss to follow up, blow out in specialist wait times and increased admin burden.”

Multiple Sclerosis vs Antibody Disease – What GPs Need to Know

Using SGLT2 to Reduce Cardiovascular Death in T2D – Important Updates for GPs

Menopause and MHT: Maximising Benefits & Minimising Risks

Peripheral Arterial Disease

Yes
No
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
