Articles / 60% of GPs would back more UCCs, if…

A Healthed poll this week found 65% of 1200 GP respondents are supportive of UCCs in general.
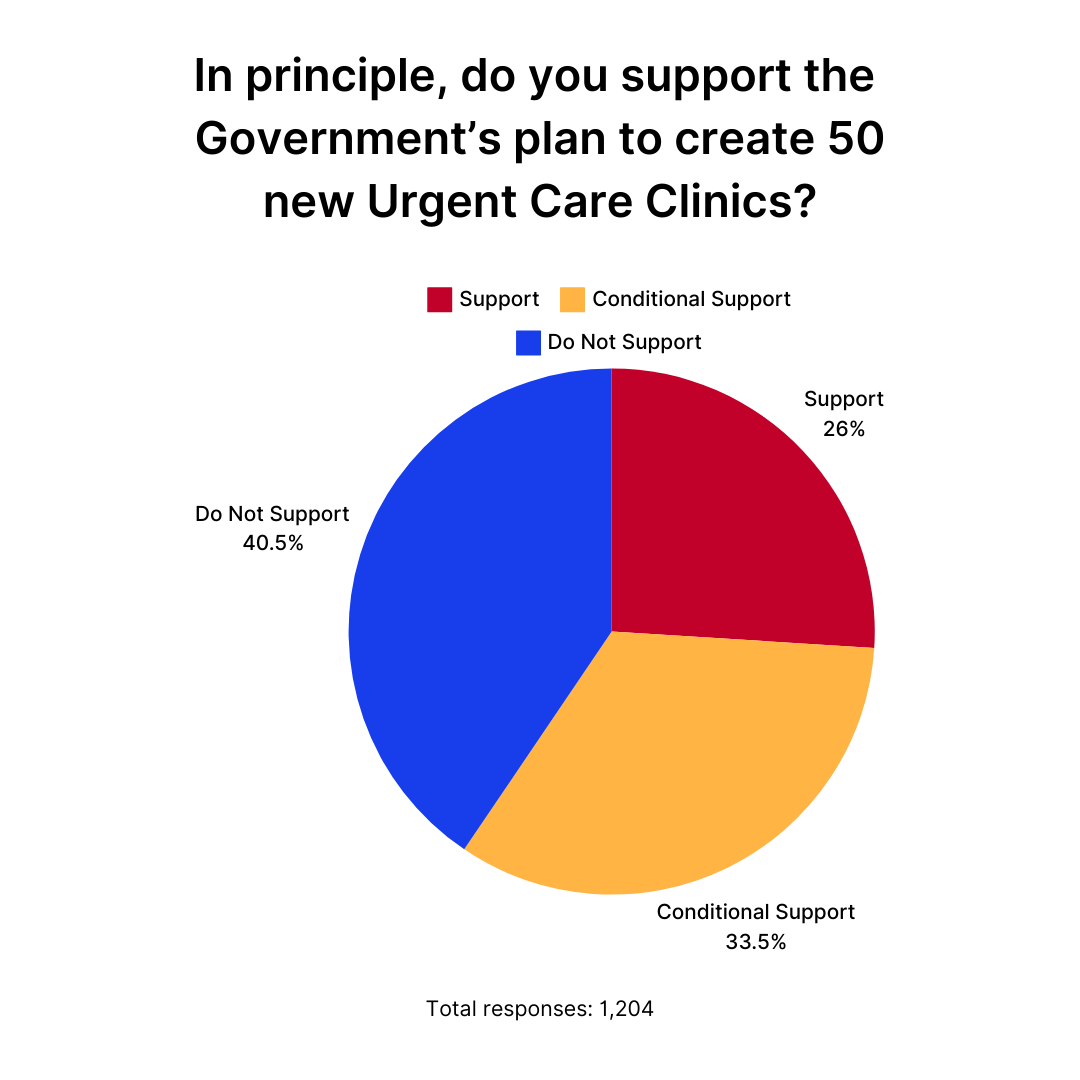
But when it comes to the Government’s latest election promise to add 50 more clinics by mid-2026, only about one quarter of GPs support the initiative outright, while one third say that while they support the idea in principle, modifications are needed – and 40% say they oppose the new clinics.
Concerns about continuity of care, staffing issues, cost effectiveness, triaging and lack of evaluation were common among those who believe modifications are needed — and those who don’t support UCCs at all.
“Economic outcomes need to be evaluated. The clinics should have strict triage criteria to avoid incomplete patient care for conditions that are NOT urgent, and to avoid fracturing continuity of care with their GP,” one GP commented.
The College has been particularly critical of the plan.
“The announcement means more than $1 billion has now been allocated on establishing these clinics in every state and territory, despite no evidence showing their effectiveness or efficiency,” RACGP President Dr Michael Wright wrote to members on Sunday.
“We don’t know whether they’re providing value for money, or even if they’re keeping patients out of hospital emergency rooms.” – Dr Michael Wright
“The other worrying element seemingly being ignored by government is that some of the existing UCCs are already closing because they can’t find anyone willing to work in them,” Dr Wright added.
Several GPs in Healthed’s survey echoed this concern.
“Every time the government does this, they can’t get staff and it ends up being an allied health clinic,” one GP commented.
“The proposal is bound to de-staff general practice,” another worried.
Many who expressed conditional support for UCCs said they are best suited to rural and regional areas.
“It needs to really be located in areas of need, not in marginal seats,” one GP quipped.
“I support UCCs in rural areas where it is difficult to get a GP appointment immediately and it is either that or go to emergency. There is no point in metro areas. There are plenty of clinics that are open and available after hours. In the end the regular GP is stuck sorting out the matter the next day,” another GP commented.
“It would be best if urgent care clinics could be co-located near existing emergency departments,” suggested another.
Better follow-up care is also crucial, GPs said, with several noting that measures such as discharge summaries and sending results to GPs is crucial.
“I think they should be a part of usual GP clinics to ensure continuation of care, opportunistic preventative care and allow transfer of information to be readily accessed,” one GP suggested.
“These clinics need to get a copy of the doctors consultation notes to the patient’s own GP or get a copy uploaded to mygov…,” another GP wrote.
“They must operate purely for urgent care, avoiding an unnecessary ED presentation, with a letter sent to their regular GP, outlining treatment given,” another GP commented, adding “They should be located only in areas of need.”
“Previously super clinic were implemented, but then it turned out to be like any private practice, not accepting patients or opening after hours. Hope there will be more regulatory and strict measures for them to apply what they are supported to do.”
“It needs to be very clear what the Urgent Care Clinics should be treating, as it is fracturing primary health care and prevention. If it is not rolled out properly with clear messaging for patients (and doctors) then it will result in short term gains with shorter wait times in ED, however long-term poorer health outcomes for patients…”
“In principle it is offering patients some availability to GPs at odd hours when usual GP not available. But my patients have complained of long waiting times and still needing to be referred to tertiary hospital.”
“Patients need choices for urgent but not life-threatening conditions, but there is no continuity of care and therefore often quality of care suffers and the end result is not cost effective>”
“Urgent care clinics would be helpful if they were attracting patients who would otherwise go to Emergency. However, they seem to be taking GPs from existing practices and seeing patients who would otherwise go to a GP. Improved funding of GP would be of more benefit.”
“Urgent clinics should be extension of hospital emergencies with clear communication with local GPs.”
“I have mixed feelings, but given many GPs prefer to not work full time, or do after hours work, I think these clinics have a use. Equally they pull doctors away from GP sessions.”

An Update on Heart Failure in Primary Care

Allergen Introduction – Practical Tips for GPs

Falls Prevention – A Practical, Evidence-Based Update on What Really Works

Vulvovaginal Health – From Childhood to Menopause

Very overestimated
Moderately/slightly overestimated
Quite accurate
Moderately/slightly underestimated
Very underestimated
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
