Articles / ‘It’s complicated’ – UCCs fill a gap, but who’s paying for it?

Last Sunday, the Government announced another 50 fully bulk billed Medicare Urgent Care Clinics would be set up by mid-2026, at a cost of $644 million if Labor wins re-election – bringing the total investment in UCCs to over $1 billion.
We don’t know, experts say. Health economist and University of Melbourne Professor Stephen Duckett is on the advisory committee to the consultants who are evaluating UCCs – but there is no date set for either the interim or final reports, he says.
“We know anecdotally that people are going to UCCs who would otherwise go to emergency departments. But that’s all anecdote,” he says. “We have to wait to fully evaluate the UCCs.”
We do know that UCCs are estimated to cost about $200 per head, which while cheaper than an ED visit, is more than four times the cost of a standard GP appointment.
Professor Charlotte Hespe, a GP and academic who specialises in improving health outcomes through general practice, says they are Band-aid solution with a hefty price tag.
“Each consultation is funded at a much higher rate than a standard consultation, which is one of the arguments that the RACGP has. Why would you be funding urgent care clinics proactively over general practice when it’s costing $200 per consultation versus $42?” she asks.
Professor Karen Price, also a GP and researcher, and past President of the RACGP, agrees.
“I would like to see the name changed and call it for what it is, heavily subsidized general practice in marginal electorate seats,” Professor Price says.
“I don’t like the way that the Government’s politicking about this, because they removed after-hours funding from general practice years ago, and then they’re surprised that there’s no after-hours care or extended care. Then they prop up another avenue of care that fragments general practice continuity,” she says.
The College has railed against Labor’s plan – but GPs have offered tacit support.
Sixty five percent of GPs said they support UCCs ‘in principle,’ according to a Healthed survey of more than 1200 respondents – but their views on the most recent announcement to add 50 more of these clinics were more nuanced.
GPs commented that UCCs could play a role in rural and regional areas of need, but expressed concern that they come at the expense of adequate investment in general practice, will be difficult to staff, and jeopardise continuity of care.
So what gives?
“I think when GPs say they’re in support of it, they do want their patients to have access to care. Of course they do, we all do. We’re all in support of a high-functioning health system – the question is whether or not this is it,” Professor Price says.
The RACGP, and many of general practice’s most outspoken voices, argue that it isn’t.
“Colleges are in support of patients getting after-hours care, but integrated into usual general practice care,” Professor Price says, noting that when she started as a GP, it was common to work after hours, occasional weekends and sometimes even overnight, “because there was funding available.”
Not so anymore.
“They change the system, then complain the system doesn’t work, and then they reinvent it again, but in a slightly more clunky way,” Professor Price sums up.
“It was actually their broken system in the first place. So can we just get down on with the reform and, less about winning votes and making yet another band-aid on an already very injured patient.”
Professor Hespe notes that while UCCs offer a short-term quick fix, they likely cost us more in the long run than properly investing in GP.
“Some things might be triaged as a level 4 or 5, but it has to be, because of the care and the investigations that need to be done, it actually is a hospital service that’s required to sort it out versus some things like fractures and sutures and things like that can easily be done in a GP setting,” Professor Hespe says.
“So it’s a very blurred line between some of these things that don’t need to go into a hospital for, versus what can be dealt with in an urgent care centre, versus should really be being seen by the usual GP.”
As the government pours money into urgent care, there’s always the question of where else it could be used. Professor Duckett says its too simplistic to say money that’s allocated to urgent care is money that would have gone to Medicare – it could go to any policy, but it does come at a cost.
“The Government makes a trade-off between whether it’s going to put extra money into urgent care centres or extra money into tripling the bulk billing incentive or extra money into more nuclear submarines or whatever,” he says.
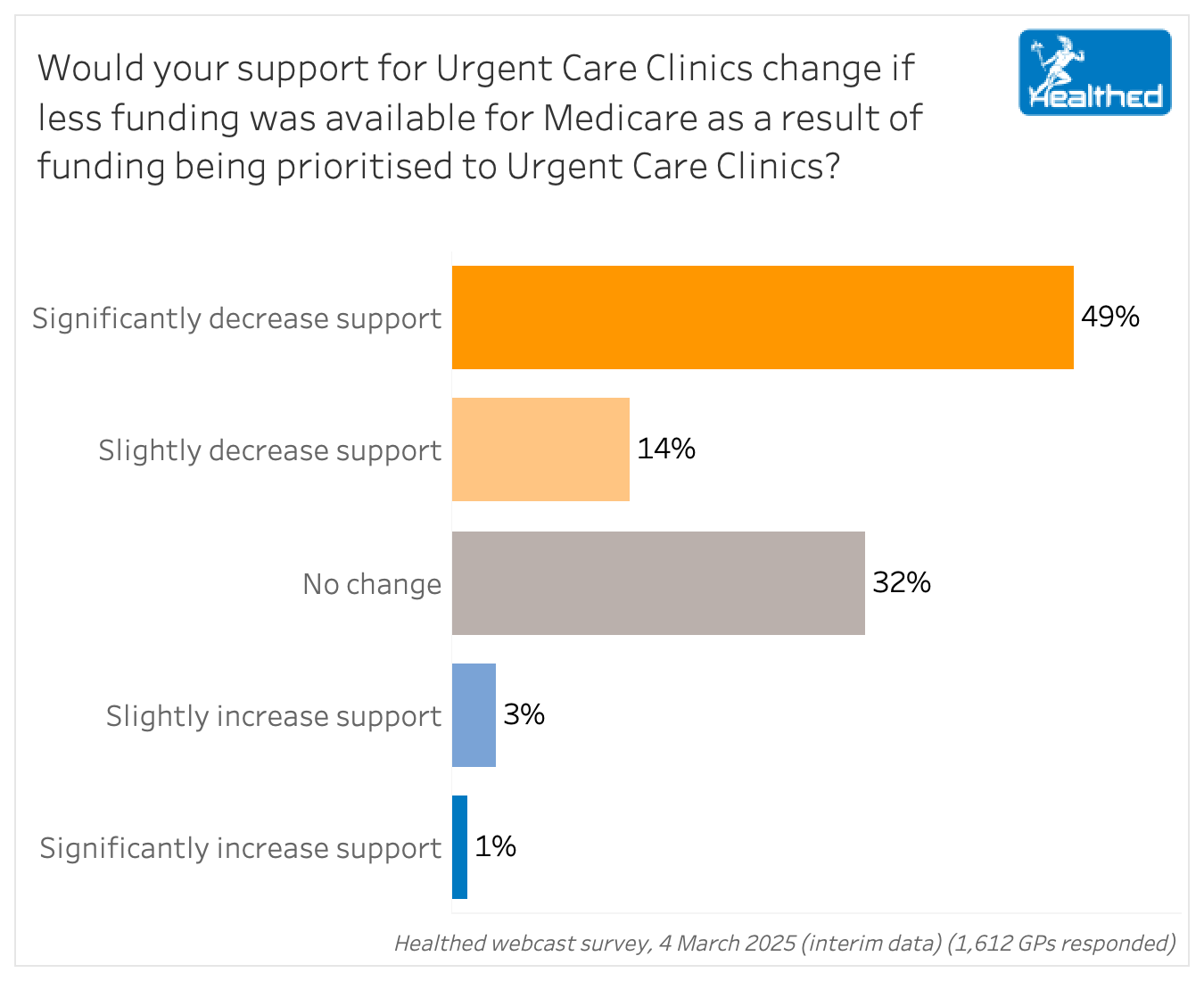
Framed that way, GPs in Healthed’s survey said if less funding was available for Medicare as a result of prioritising urgent care clinics, they would be significantly less likely to support UCCs.
“The philosophy from the RACGP is that if you look at the data, continuity care actually saves more money down the track than any other strategy,” Professor Hespe says.
“So the provision of yet another siloed care system outside of general practice is actually not going to solve this problem long-term, nor is the issue about how do we deal with the fact that Medicare no longer is funded at a level that means that GPs can provide that care in the community without a gap fee being paid.”
Professor Henry Cutler, director of Macquarie University’s Centre for Health economy, argues in the Conversation that cost and waiting times are important factors in patients’ choice to seek urgent care or emergency care, with some research suggesting people use urgent care to avoid gap fees and long waits for a GP.
This is a point Professor Hespe makes too.
“If I’ve got an urgent ‘healthcare need’, I will put off seeing my GP because I’m having to pay a gap, whatever that might be, whereas if I go straight to the emergency department, it is free. And so we have this dilemma. We have people who are putting off things that could be managed non-urgently that then end up being urgent and going into the emergency department,” she says.
“Everybody gets that Medicare is needing to be redesigned. So can we just do that instead of continuing to prop it up? Band-Aid on top of Band-Aid is still not doing anything.”

Allergen Introduction – Practical Tips for GPs

Oral Contraception Update

What do we do With High Triglycerides?

An Update on Heart Failure in Primary Care

Very overestimated
Moderately/slightly overestimated
Quite accurate
Moderately/slightly underestimated
Very underestimated
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.





