Articles / Age-related macular degeneration: expert tips to improve outcomes

0 hours
These are activities that expand general practice knowledge, skills and attitudes, related to your scope of practice.
0.5 hours
These are activities that require reflection on feedback about your work.
0 hours
These are activities that use your work data to ensure quality results.
These are activities that expand general practice knowledge, skills and attitudes, related to your scope of practice.
These are activities that require reflection on feedback about your work.
These are activities that use your work data to ensure quality results.
Age related macular degeneration (AMD) affects one in seven people over 50 and is often asymptomatic in the early stages. So it’s important to encourage people to have their eyes tested at least every two years, says retinal specialist Associate Professor Alex Hunyor, board member of Macular Disease Foundation Australia and chair of its medical committee.
The key feature of AMD is central vision disturbance, as opposed to generalised visual disturbance, he says.
Specific symptoms include:
Refer urgently if any of these symptoms develop suddenly, as they are suggestive of neovascular (wet) AMD, Associate Professor Hunyor says.
“Any patients presenting with sudden vision changes should be seen within a few days by an optometrist or ophthalmologist, as early diagnosis and treatment of neovascular AMD is essential to obtain the best possible results.”
Symptoms may start in one eye, especially in acute AMD, so ask patients to test each eye separately, by covering one eye and then the other – as is done when testing visual acuity, Associate Professor Hunyor says.
While people may describe specific central visual symptoms, they will often use more nonspecific terms such as blurry vision, problems reading, or thinking their glasses are dirty, but the vision problem is still there when they clean their glasses, he adds.
“Sometimes people will notice a problem incidentally when they rub or cover one eye and find that the other eye has poorer vision. It is common for conditions like AMD to present with unilateral symptoms, and unless people close or cover the other eye they often do not notice even quite marked visual reduction as the good eye compensates,” Associate Professor Hunyor says.
As the condition progresses patients frequently have difficulty reading number plates and street signs and recognising faces.
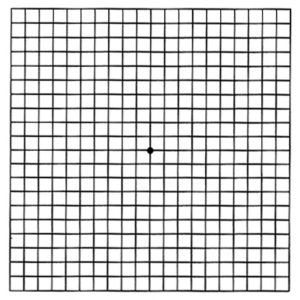
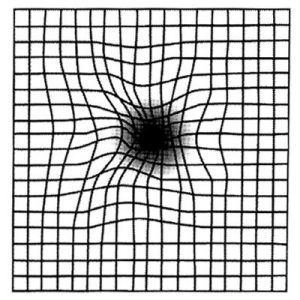
The Amsler grid, pictured below, can help detect central visual disturbance. You can find free printable versions of the Amsler grid eye test to show patients—and patients who have AMD can self-test at home using a free Amsler grid app.
The first image below shows a normal Amsler grid, while the second one shows how it would typically appear to someone with acute onset neovascular AMD.
Figure 1: Amsler grid
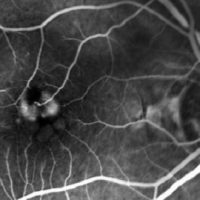
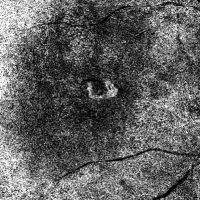
Specialised tests are used to confirm the clinical diagnosis of neovascular AMD. Most commonly, optical coherence tomography is used to demonstrate signs of leakage from the abnormal vessels under the retina (figure 2). Retinal angiography may also be used in selected cases (figure 3).
Figure 2: Neovascular AMD
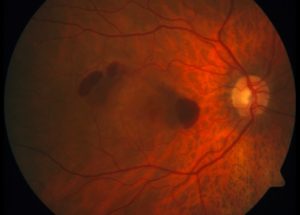
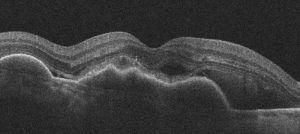
Figure 3: Retinal angiography
Age is an important nonmodifiable risk factor––with the risk of developing AMD increasing more than threefold in those over 75 years compared to those between 65 and 74—as is family history, Associate Professor Hunyor says.
“If an individual’s parent or sibling has AMD, there is a 50% chance of the individual developing AMD. Those with a family history of AMD should be made aware of this risk and be encouraged to have regular eye health check-ups.”
Smoking is the strongest modifiable risk factor for macular degeneration.
“Increasing pack-years of cigarettes smoked is directly linked with an increased risk of AMD and associated with a 10-year younger age of onset, bilateral disease, and a two-fold increase in risk of developing late AMD,” Associate Professor Hunyor says.
Patients with known AMD who smoke should be strongly encouraged and assisted to quit, he adds.
Eating patterns and nutrition are also important, and Macular Disease Foundation Australia recently released new nutrition guidelines to reduce AMD risk and/or slow its progression.
Treatment protocols with intravitreal anti-VEGF injections for neovascular AMD are well established, Associate Professor Hunyor says, with four agents on the PBS: ranibizumab, aflibercept, brolucizumab and faricimab.
“Early treatment is the key to maintaining (and in some cases improving) vision in the short term, and reliable persistence with treatment is essential for the benefits of treatment to be maintained.”
Customising treatment intervals
“Modern treatment protocols focus on maximising visual results and customising treatment intervals to reduce the burden of clinic visits,” he says.
The initial treatment interval is 4-weekly for the first 3 injections. After that the treatment interval is customised to the individual according to disease activity.
“On average, patients need 7 injections per eye in the first year and between 5–7 injections each year after that, often for the rest of their lives,” Associate Professor Hunyor explains.
“Some patients will be able to have their treatment interval extended out as far as 16 weeks.”
“Unfortunately, 20% of people will stop treatment by the end of the first year, and 50% of people will stop their eye injections within five years,” Associate Professor Hunyor says.
Generally, if patients stop injections their visual prognosis reverts to that of untreated disease.
“Patients often feel that they are not benefiting from treatment because their vision is not improving, but stable vision actually indicates treatment success, as their vision would usually deteriorate markedly without treatment,” he says.
Explaining this can encourage patients to persist with treatment, he adds.
One way to illustrate the stakes is to show patients the 6/60 letter at the top of the vision chart, and explain that without treatment, they would have over 50% chance of not being able to see that largest letter within two years.
He also suggests explaining why it’s important to stick to recommended treatment intervals; if they don’t, blood vessels will become active and may cause more damage to the macula.
If they do miss appointments or say they want to discontinue treatment, he suggests asking why, and letting the specialist know. The Macular Disease Foundation’s Eye Connect program also provides support and information tailored to their individual circumstances.
Currently no treatments for atrophic AMD are available in Australia, although one intravitreal agent — pegcetacoplan, a complement inhibitor, was recently approved by the TGA. Numerous other agents are in clinical trials worldwide, Associate Professor Hunyor says.
“These treatments have been shown to slow the growth of atrophic lesions, however they do not reverse existing atrophy or vision loss, and have not been shown to benefit visual acuity.”
Note: This article was first published on 5 July 2024. It has been updated and reviewed by Associate Professor Alex Hunyor in August 2025.
Based on this educational activity, complete these learning modules to gain additional CPD.

Allergen Introduction – Practical Tips for GPs

Oral Contraception Update

What do we do With High Triglycerides?

An Update on Heart Failure in Primary Care

Very overestimated
Moderately/slightly overestimated
Quite accurate
Moderately/slightly underestimated
Very underestimated
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.





