Articles / ‘CALD’ women less likely to get cervical screening

Despite Australian women having among the lowest incidence and mortality rates for cervical cancer in the world, some groups remain at higher risk than others.
More than 70% of cervical cancer cases in Australia occur in people who have either never been screened or are overdue for screening.
Women from culturally and linguistically diverse (CALD) backgrounds are less likely to participate in cervical screening than those born in Australia, and available data shows that those from some CALD backgrounds also have higher cancer rates, says Professor Marion Saville, AM, Executive Director at the Australian Centre for the Prevention of Cervical Cancer.
The Federal Government’s push to eliminate cervical cancer in Australia by 2035 includes strategies to promote cervical screening to CALD women, but what is the state of play in practice right now?
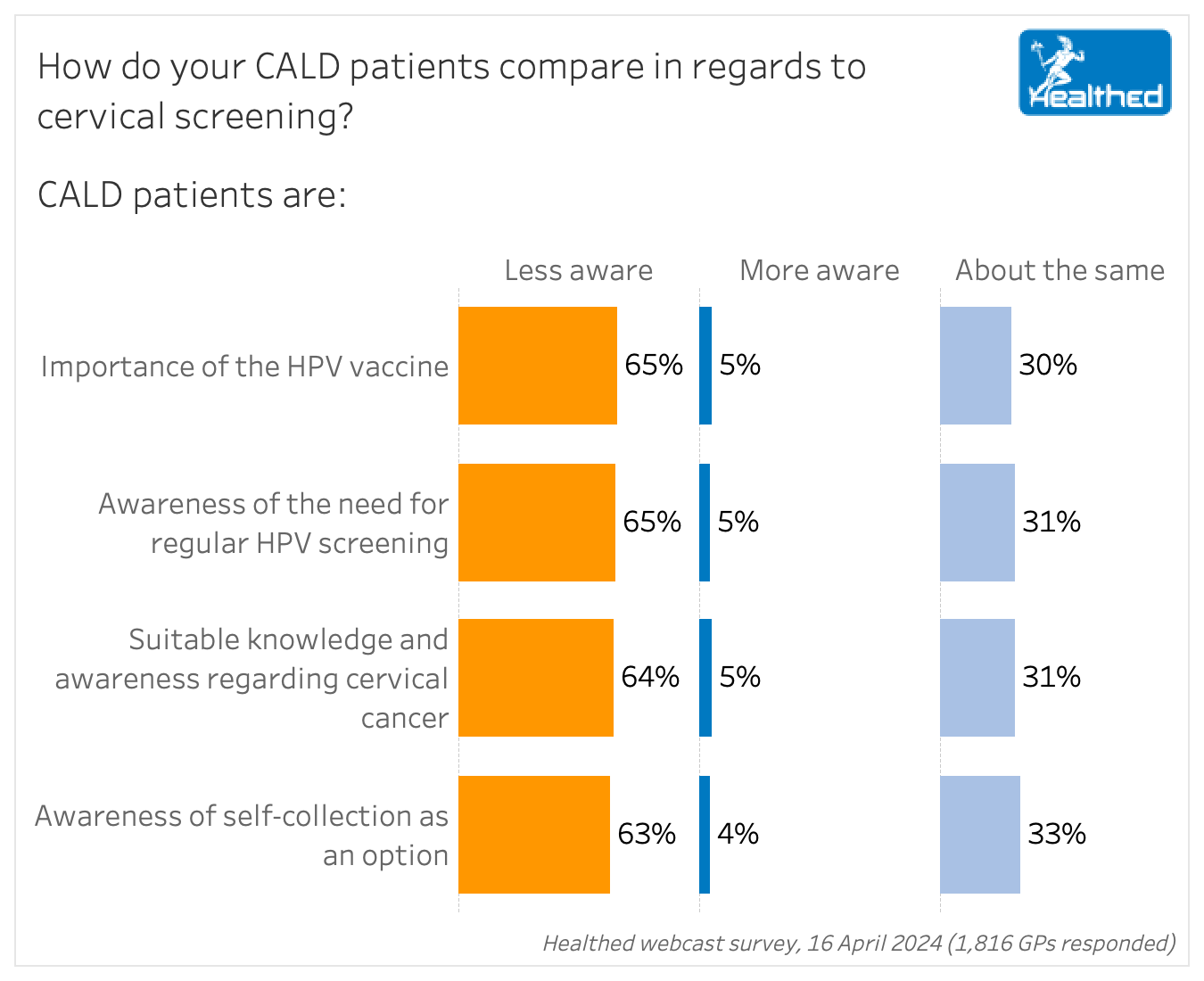
About two-thirds of GPs believe their CALD patients are less aware of issues surrounding cervical cancer, including the option to self-collect a vaginal sample for screening, a recent Healthed survey found.
According to the latest National Cervical Screening Program report, uptake of self-collection has increased consistently since the option was extended to all women, including in never- and under-screened people.
The biggest increases have been seen in 70–74-year-olds, the Northern Territory, very remote areas, and among those who are most disadvantaged.
The report notes there is currently not enough data to accurately analyse participation rates of culturally and linguistically diverse women — while country of birth and main language spoken at home other than English have been added to the National Cancer Screening Register, these fields haven’t been filled out for most participants.
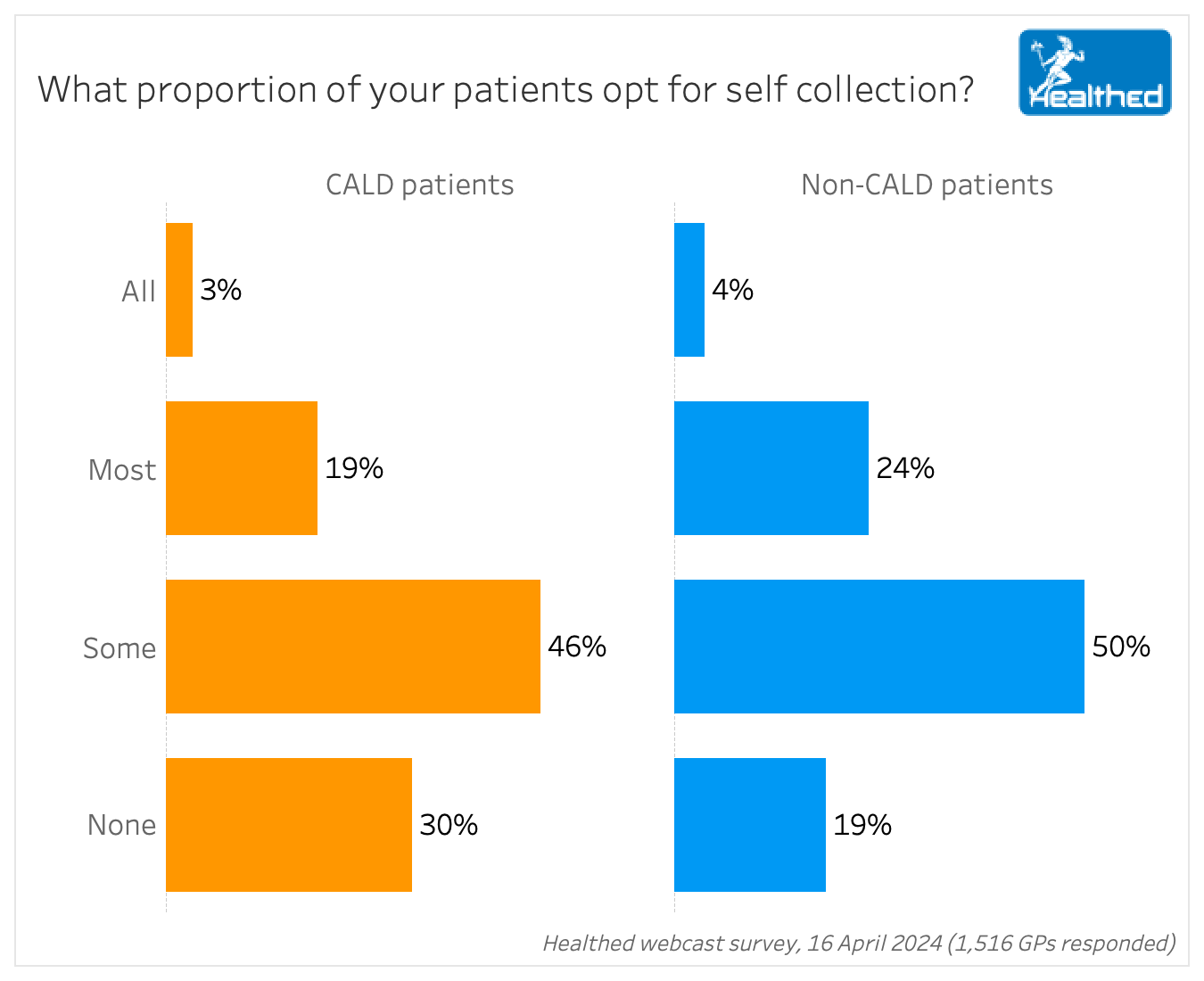
In Healthed’s 16 April survey, GPs asked to estimate the proportion of their CALD versus non-CALD patients who opt for self-collection reported that their non-culturally and linguistically diverse patients were slightly more likely to choose self-collection than their more diverse counterparts.
Eliminating the need for a speculum examination makes screening more accessible to many under-screened patients, Professor Saville says.
She stresses that GPs play a key role in breaking barriers to cervical screening.
“Discussing the option to self-collect with all eligible patients is extremely important. I would highly encourage GPs to make sure they offer both tests and explain the process of both to their patients,” she says.
A 2022 Australian descriptive study involving 12 GPs found facilitators to screening in CALD women included a continuing doctor–patient relationship, initiating the discussion about screening, and the availability of self-collection. Barriers included lack of patient awareness, the perception that screening is a low priority, and language difficulties.
Professor Saville advises GPs to give patients in-language resources if needed, noting that self-collection instructions in 20 languages can be found on the ACPCC website, and other translated resources on the National Cervical Screening Program website.
Aboriginal and Torres Strait Islander women have over double the incidence and 3.5 times the mortality associated with cervical cancer compared with other Australians, and it is known their participation in cervical screening is lower.
By removing feelings of shame, embarrassment and discomfort associated with the clinician-collected test, self-collection could help close this gap, Professor Saville says.
A 2017 pilot study led by Professor Saville conducted at an Aboriginal Health Service found 85.7% of under-screened women who declined a speculum examination provided a sample after being offered self-collection, she says. There were also high rates of follow-up for those who undertook a self-collected test.
“Patients described the self-collection process as empowering, supporting bodily autonomy, easy to do, convenient, and less embarrassing than a speculum examination,” she says.
Along with Aboriginal and Torres Strait Islander and CALD women, the National Strategy for the Elimination of Cervical Cancer in Australia lists people with disability, LBGTQ+ and intersex people, and those living in rural and remote areas as key under-screened groups for targeting the promotion of cervical screening.

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart


Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
