Articles / Budget delivers cheaper medicines and more bulk billing but leaves out long-term health reform


writer
Professor and Director, Macquarie University Centre for the Health Economy, Macquarie University
Less than two months from an election, the Albanese government last night presented a budget that aims to swing the voting pendulum its way.
Headline health expenditure includes:
These announcements were already strategically made over the past month to maximise media coverage and build election momentum.
Australians want more access to affordable health care – and the budget delivers this for many. But it doesn’t push the process of health reform forward, which is needed to secure the health system’s long-term sustainability.
While the budget contains large health expenditure items, a significant amount was not strictly new funding, but already provided for by the government.
Consequently, the budget only allocates an additional $7.7 billion to health compared to actual spending for 2024-25.
This increase aligns with steady long-term spending trends from previous years. It reflects a 6.6% increase in nominal spending (when inflation is included), but only a 3.9% increase in real spending (when inflation is taken out).
Actual and estimated expenditure from the health portfolio
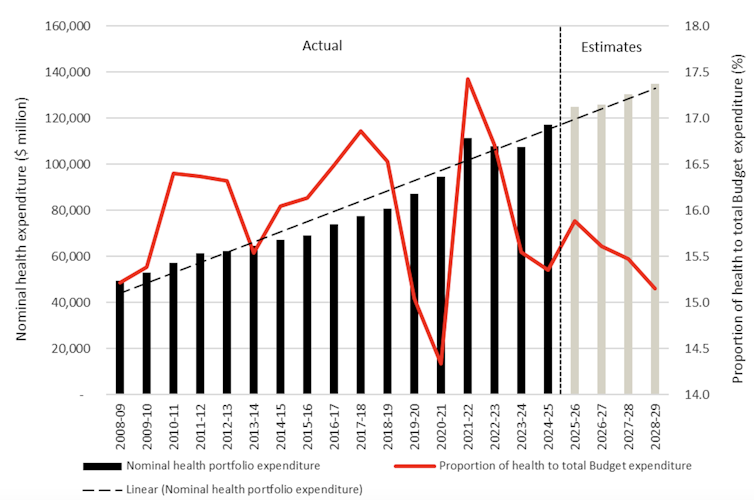
The proportion of the budget spent on health could be considered historically low, projected to be 15.9% for 2025-26.
It’s unclear whether Australians want more of the budget allocated to health, but there is certainly a need for greater investment.
The Albanese government is trying to kill three birds with one stone with this health budget. It wants to reduce the cost of living, improve health outcomes, and win an election.
Keeping the cost of living down and improving health services are the top two most important issues for this election. Headline health announcements directly address these two issues.
However, they also deliver a political benefit by shifting the media spotlight away from Opposition leader Peter Dutton. He was unable to legitimately counter attack headline health announcements given his unpopularity when he was a health minister. Instead, he promised to match some health announcements if elected.
Increasing bulk-billing rates and reducing prescription prices will directly reduce out-of-pocket costs for many Australians. This will mostly be for people without a concession card.
Increasing access to urgent care clinics will also help reduce cost of living pressures because they deliver services free of charge.
Making health care cheaper for patients will also improve health outcomes. Many Australians sometimes choose not to access health care because of its cost, which can lead to worse health outcomes and expensive hospital care.
The magnitude of any health improvement will depend on how patients respond to cheaper health care.
More health benefit will go to patients who start seeing their GP rather than staying at home and trying to manage their condition themselves.
The health benefit will be less for patients who start seeing their GP instead of an emergency department or urgent care clinic, because they are substituting one place of care for another.
There is an “opportunity cost” every time the government spends money. Using the health budget to reduce the cost of living means less money to improve the health system elsewhere.
In that context, this health budget has missed an opportunity to build a more sustainable health system.
Medicare is not the best way to fund community care from GPs, nurses and allied health providers. It imposes barriers to establishing seamless multidisciplinary team-based care. These include restricting the types of services non-GP clinicians deliver, and not funding enough care coordination. People with chronic disease, such as diabetes and heart disease, often fall through the cracks and become sicker.
A review of general practice incentives submitted to the health department last year recommended transition towards new funding models. This could include funding models that pay for a bundle of services delivered together as a team, rather than a fee for every service delivered by each team member.
But payment reform is extremely hard. Medicare has not substantially changed since 1984 when it was first introduced.
Given this budget allocated $7.9 billion to increase bulk billing alone, and $2.4 billion ongoing, this budget has a missed opportunity to start the payment reform process. This extra funding will reinforce current payment structures, and could have been used as leverage to get GPs over the line on reforming Medicare.
The government also missed an opportunity to start reforming the health workforce. An independent review, also submitted last year, sought to improve access to primary care, improve care quality, and improve workforce productivity.
It outlined 18 recommendations, including payment reform, to remove barriers to increase access to care delivered by multidisciplinary teams of doctors, nurses and allied health providers such as psychologists and physiotherapists.
Again, there was nothing in this budget to suggest this will be pursued in 2025-26.
What next usually depends on which party wins the election.
In this case, Dutton has agreed to match the health budget spending on bulk billing and price reductions for PBS scripts. But the Coalition has not committed to 50 more urgent care clinics.
Whichever party wins, there is an urgent need to substantially reform health care if our health system is to remain one of the world’s best. ![]()
Henry Cutler, Professor and Director, Macquarie University Centre for the Health Economy, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
![]()

Allergen Introduction – Practical Tips for GPs

Obstructive Sleep Apnoea

writer
Professor and Director, Macquarie University Centre for the Health Economy, Macquarie University

Very overestimated
Moderately/slightly overestimated
Quite accurate
Moderately/slightly underestimated
Very underestimated
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.





