Articles / Burnout impact looms large, survey suggests


writer
General Practitioner; Author; Past Chairman, RACGP; Past Deputy Chancellor, Monash University
0 hours
These are activities that expand general practice knowledge, skills and attitudes, related to your scope of practice.
0 hours
These are activities that require reflection on feedback about your work.
0 hours
These are activities that use your work data to ensure quality results.
These are activities that expand general practice knowledge, skills and attitudes, related to your scope of practice.
These are activities that require reflection on feedback about your work.
These are activities that use your work data to ensure quality results.
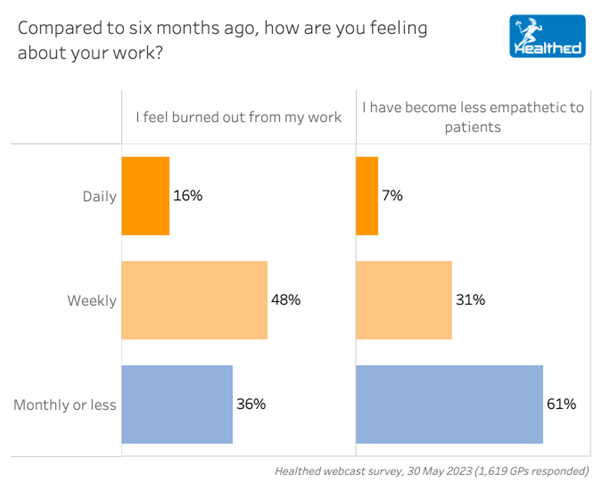
The results of a Healthed survey of more than 1600 GPs last month show just how widespread burnout and its impact are in general practice, with a whopping 64% of respondents reporting that they regularly feel burned out from their work. Additionally, 38% of surveyed GPs said they’ve become less empathetic to patients on a daily or weekly basis.
According to the International Classification of Diseases 11, burnout encompasses three domains: exhaustion, cynicism and reduced professional efficacy.
Burnout may be common, but it’s not normal. It has serious consequences and should not be accepted as ‘part of the job’ or worn like a ‘badge of honour’.
In everyday life, we see it manifest as uncharacteristic irritability, reduced productivity and efficiency, and dissatisfaction with work in our patients – and ourselves.
The true extent of burnout amongst GPs is often hidden. Many continue to function at work at great personal expense, while others reduce hours or retire early, particularly if untreated burnout transitions to mental illness. Due to negative stigma deterring early treatment for mental health problems in the medical profession, many GPs tend to battle on alone or seek help late during a crisis, and unfortunately this can leave them resistant to treatment or prone to relapse.
1. Fully confront all your concerns. Try to find a few minutes of peace and a blank sheet of paper. Write down all your major and minor stressors – all those upfront concerns as well as the worries in the back of your mind. Rather than avoiding your issues, confront them full on. Embrace your emotions, including the unpleasant ones. Remember to acknowledge pandemic pressures – COVID-19 is far from over. Reassure yourself that you have every reason to feel stressed when you review your long list of issues.
2. Accept that life is challenging. There will always be issues you cannot fix. There will always be too many things on your list of issues. You are human – not superhuman. Try to accept what you cannot change, and instead, identify the issues you have influence over. Schedule a future time to address work issues with like-minded colleagues when you are thinking clearly.
3. Float above your thoughts. Try to observe your thoughts from afar to give your brain a break. Your time off work is a precious opportunity to nurture and rejuvenate yourself. Doing nothing and feeling bored on your time off may initially feel unpleasant, but try to accept this as positive – it means your mind is slowing down. You are not your thoughts – try to float above your thoughts.
4. Let time heal. As there is a complex biological basis for burnout, you may not feel better immediately with relaxation and rest. Be patient with yourself. While you are waiting for your stress hormones to settle, bask in love and reconnect with people who provide mutual support and energise you. You will feel better in time.
What doesn’t help is allowing negative thinking to fester on your precious time off work. Your unhelpful inner voice may ask: ‘What’s wrong with me?’ ‘Why can’t I cope?’ ‘Am I not cut out for this?’ ‘Should I leave general practice?’
It can be overwhelming worrying about issues you cannot influence or potential future problems which may never manifest. Try instead to reassure yourself that it takes time to unwind, relax physically and enjoy slowing down. Do not make major life decisions about your career when you are mentally exhausted.
It’s not at all surprising that burnout in general practice is at a record high – GPs are continuing to respond to surges in COVID-19, and the fall out of late diagnoses of serious non-COVID-19 conditions and a mental health crisis in our communities. Since the pandemic, the whole health system is cracking under excessive prolonged pressures.
After a mentally and physically exhausting week at work, are you taking steps to reduce stress and protect yourself from burnout?
Don’t underestimate how important it is to seek informal debriefing with a trusted
colleague, family member or friend to help. Simple actions such as connecting with people who love you, physical activity in the fresh air and/or mindfulness and relaxation techniques can help enormously.
If these strategies don’t help, please consult an independent treating GP, psychologist or psychiatrist for an objective assessment. Self diagnosis and self treatment are inadequate. Please take care and seek support.
Adapted from ‘Every Doctor; healthier doctors=healthier patient’ coauthored by Prof. Leanne Rowe AM, Dr Vihangi Abeygunawardana, Prof Michael Kidd AO, published internationally by Taylor and Francis | www.everydoctor.org
Ref:
1. Based on the work of Dr Clare Weeks MBE, The Latest Help for Your Nerves (1989)

RSV Prevention in Infants and Pregnant Women

STIs – Common and Tricky Cases

Role of Testosterone During Menopause - Evidence vs Hype

Vision and Driving Fitness: Key Insights for Health Practitioners

writer
General Practitioner; Author; Past Chairman, RACGP; Past Deputy Chancellor, Monash University
Yes
No
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Notifications