Articles / CPD-induced retirements

Thirty percent of GPs say they are bringing forward their retirement plans, thanks to the new CPD system changes introduced 15 months ago — with more saying they are making plans to leave general practice, if not retire completely, according to a national Healthed survey of more than 2200 GPs.
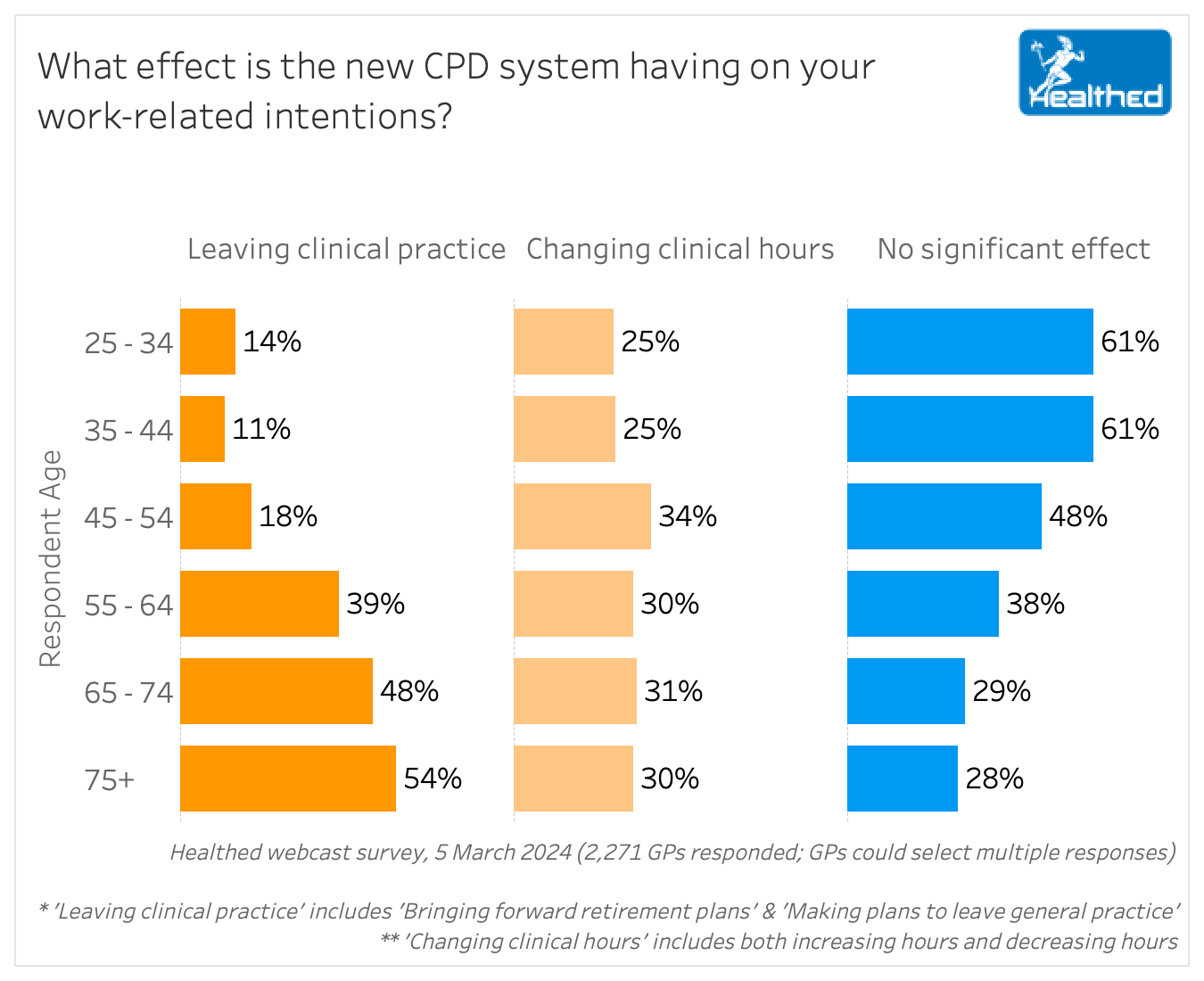
Not surprisingly, older GPs are much more likely to be planning an early exit.
Just 16% of GPs under age 55 said they are bringing forward retirement plans or otherwise planning to leave general practice as a result of the new CPD system, compared with 45% of GPs over age 55.
Dr Mukesh Haikerwal, a Melbourne GP and chair of the Australian GP Alliance (AGPA) says the survey results echo feedback the AGPA is consistently hearing.
“It’s a major pain point for the profession,” Dr Haikerwal said. “People are very upset about the complexity of what they’re being asked to do, and also the time demands of it in the current format, so what you’ve uncovered is completely in keeping with what we’re being told.”
Dr Haikerwal said the intrusive CPD is adding yet another layer, causing people to reconsider continuing in the profession, “and to be honest, the ones that are most likely to go are the ones we want to keep at the moment,” given the shortfall of both doctors established in the workforce, and doctors coming through to replace them.
“Until we get an even throughput, a pipeline, we should try and maintain people and make it something they’re comfortable and confident to do — not make it more difficult and cumbersome and therefore something that they want to avoid and leave early,” Dr Haikerwal said.
Yet when Healthed asked the Medical Board what could be done to mitigate the impact of CPD on the workforce shortage, little in the way of tangible solutions were offered.
“Medicine is a challenging and rewarding profession and every doctor has the right to decide when to stop contributing to their community as a medical practitioner,” Chair of the Medical Board Dr Anne Tonkin said.
“There is no question that right now, workforce shortages and patient needs are out of sync and this is increasing the pressure on doctors, especially GPs,” Dr Tonkin said, noting that the Board is working to find regulatory solutions to ease workforce pressures.
However, she downplayed the likely impact of CPD change.
“There is rarely a single driver for our big life decisions like retirement. Usually, people make their decision to retire over time and after careful consideration of all the contributing factors,” she said.
“We accept that some experienced doctors have decided they did not have the energy to meet a new set of professional challenges introduced by the new CPD arrangements. We respect their decision, are grateful for their past contribution and wish them well. It’s also important to remember that patients expect their doctors will stay up to date throughout their working lives – which is the core purpose of CPD.”
Dr Haikerwal was unsurprised at the Medical Board’s response, but implored them to “take these genuine concerns seriously,” citing the onerous time commitment and impact on part-timers in particular. “Of course people need to keep up to date, and it’s part of your professional responsibility – but there is a genuine need to review.”
Dr Ramesh Manocha, CEO of Healthed, said part of the problem is that the CPD homes are disincentivised to push back on the Medical Board.
“You’d assume that the various Colleges such as the RACGP and ACRRM would be vigorously representing their members’ views on the new CPD system to the Board,” Dr Manocha said. “However, now that these Colleges have become CPD homes, they are beholden to the Board which now has the power to approve or deny their revalidation.”
“This creates a conflict of interest because if they annoy the Medical Board by campaigning to reform the CPD system, there is always the unspoken threat that the Board might not renew their status as CPD homes. So I wouldn’t be placing my hopes on the Colleges becoming the main drivers of CPD reform,” he added.

Allergen Introduction – Practical Tips for GPs

Obstructive Sleep Apnoea

Very overestimated
Moderately/slightly overestimated
Quite accurate
Moderately/slightly underestimated
Very underestimated
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.





