Articles / Focal therapy for prostate cancer


writer
Urological Surgeon; Director of Urology, Alfred Health, Melbourne
Standard curative treatments of localised prostate cancer – radical prostatectomy or radiotherapy – treat the whole prostate gland (1). These treatments are highly effective when the cancer is truly contained within the prostate. But because of the gland’s anatomical location right in the midst of such important structures – erectile nerves, urinary sphincter, bladder, rectum – injury to them is common, leading to side effects that can cause a major impact on patients’ quality of life. Add on top of this the uncertainty about which prostate cancers even need any treatment at all, and there’s a genuine risk that the treatment may harm a patient more than the disease itself.
Minimising risk of harm is a top priority. In patients with localised prostate cancer, this is attempted in several ways: by not treating low grade prostate cancers and instead keeping them under active surveillance; or in higher grade cancers, by performing erectile-nerve sparing techniques when performing prostatectomy; or by technologies that conform radiation dose more accurately to the shape of the prostate. Despite these advances, when standard treatment of localised prostate cancer is applied, erectile dysfunction, and urinary and rectal symptoms remain common. In their decision-making, patients are then faced with balancing the risk of cancer progressing by avoiding treatment versus the risk of loss of significant quality of life by going ahead. Could there be a middle path?
Focal therapy for prostate cancer is where the cancer tumour is destroyed (ablated), but the remaining healthy prostate tissue is preserved. It’s the same oncological principle as the now long-accepted standard treatment of lumpectomy for early breast cancer (2). The rationale in prostate cancer being that if tissue destruction is kept to a minimum, injury to the all-important surrounding structures will also be minimised. Evidence from studies around the world have already shown this to be true (3,4).
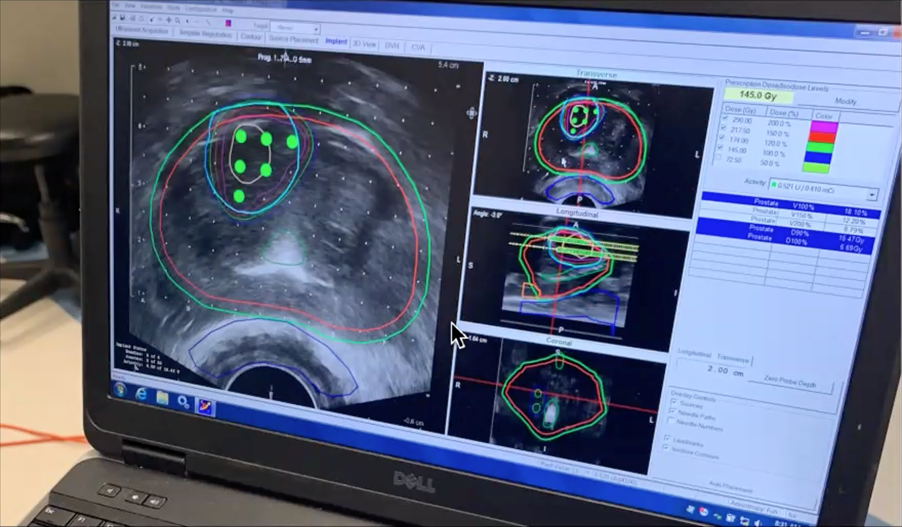
Focal cancer ablation can be achieved using various different treatment modalities or energy sources, including radiation such as brachytherapy (seed implantation – see photograph) (5), irreversible electroporation (NanoKnife) (6), HIFU (high-intensity focused ultrasound) (7), cryotherapy (8), photodynamic therapy (9) and laser (10). We don’t yet know which of these modalities is most effective, as they are all still under investigation. Various registered studies are actively recruiting in Australia now (see table) to help answer this question, as well as find out the long-term cancer outcomes.
| Study | Institution | Study ID |
| Clinical registry of focal low dose rate brachytherapy in men with biopsy confirmed low-intermediate risk prostate cancer: LIBERATE | Icon Cancer Centre, VIC | ACTRN12619001669189 |
| Hemiablative Focal Brachytherapy Pilot Study | St George Hospital Cancer Care Centre, NSW | NCT02643511 |
| Multi-Centre Registry to assess clinical and quality of life outcomes in patients undergoing the Irreversible Electroporation (more commonly known as NanoKnife) procedure | St Vincent’s Private Hospital, NSW | ACTRN12623000859684 |
| Deferral of active treatment using focal irreversible electroporation for men with localised prostate cancer | Epworth HealthCare, VIC | ACTRN12621001652864 |
| Pilot study of ProFocal-RX a novel Focal Laser Therapy device for the treatment of localised prostate cancer | Nepean Hospital, NSW | ACTRN12618001774213p |
Interest in focal therapy has skyrocketed with the recent advent of imaging (MRI and PSMA PET), which can finally reliably identify clinically significant forms of prostate cancer. These advances in imaging have led to far greater accuracy in diagnosis. The logical next step was to then apply them to precise, targeted treatment.
In theory, focal therapy sounds exactly what patients with localised prostate cancer have been desperate for – cancer cure with minimal side effects. But what might the risks be? The most obvious risk is that the cancer treated is not completely destroyed and can go on to progress locally or even spread. Another risk is that more cancer develops in the untreated parts of the prostate. And finally, it’s possible that if focal therapy fails, it could impact the ability to perform salvage treatment, such as radical prostatectomy, if scar tissue forms at the treatment site.
For these reasons, there are a few critically important points to make about focal therapy as it stands currently.
1. Patient selection is crucial
Focal therapy is a treatment for relatively small, clinically significant prostate cancers that are visible on imaging. It’s not necessary for patients with low-risk cancer, who can be safely managed on active surveillance. And it’s insufficient treatment for large high-grade cancers. Its correct application is right in the middle of these two extremes.
2. Close follow-up is essential
This consists of regular post-therapy PSA levels along with further imaging and biopsy to ensure significant cancer has been successfully destroyed. This also allows close observation of the remaining untreated prostate tissue.
3. Measuring impact through clinical trial or registry is important
Ideally focal therapy should be conducted within the setting of a clinical trial or registry, so evidence can be collected to inform all of us of the true long-term impact of this exciting new treatment option.
Professor Jeremy Grummet is a urological surgeon and Director of Urology at Alfred Health. He has been practising focal therapy since 2015 and is Co-Principal Investigator on Icon Cancer Centre’s LIBERATE focal brachytherapy clinical registry.
References:

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart

writer
Urological Surgeon; Director of Urology, Alfred Health, Melbourne


Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
