Articles / General practice as a lifestyle career? GPs weigh in…

“As a GP, you decide where you work and what hours, tailoring your workload to suit your stage of life and career. This flexibility creates opportunities to pursue other career interests, spend time with family and friends, travel, build up your savings or enjoy regular working hours,” the General Practice Registrars Australia says on their ‘Why GP’ page — while also highlighting the variety and challenge that comes with diverse patients and presentations.
The RACGP takes a more subtle approach, framing the choice around personal preferences: “When you choose to become a GP, you’re choosing a rewarding medical career that you can tailor to suit your passion, interests and life ambitions,” they tell would-be trainees on their ‘become a GP’ page.
Healthed’s national survey of more than 2400 GPs suggests this branding may be taking hold. But is that a good thing?
The majority of surveyed GPs believe younger doctors see general practice as a ‘lifestyle career’ option where they can work part time, clinic-hop, and pursue other priorities—whether that’s family, hobbies, a side hustle, or alpaca farming, as the case may be.
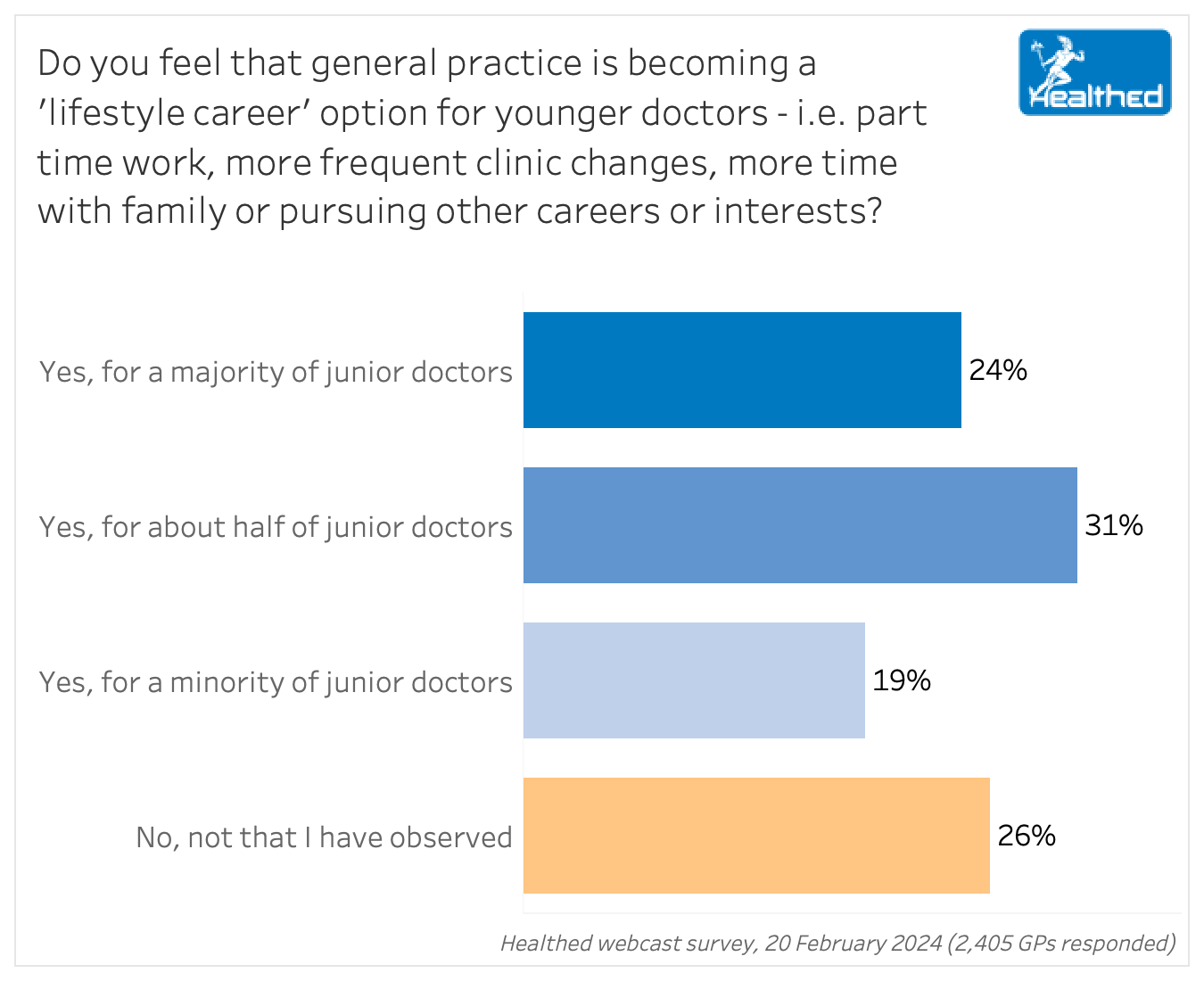
“Every doctor that we have interviewed has had work-life balance as one of the most important factors in choosing where they want to work. Not one doctor has wanted to work full-time, either male or female interviewee,” one surveyed GP noted.
The trend toward GPs working part-time earlier in their career has been reported elsewhere.
The 2023 Health of the Nation report found that 54% of GPs in training plan to be working part-time in five years. Only 34% plan to be working full-time and around 6% said they don’t plan to be working as a GP at all.
About three quarters of pre-fellowship trainees and new fellows said the promise of regular hours and quality of life had influenced their choice to become a GP — compared with 56% of mid-career GPs. The second most common factor influencing this decision, cited by 71% of trainees and new fellows, was the ability to balance family and career.
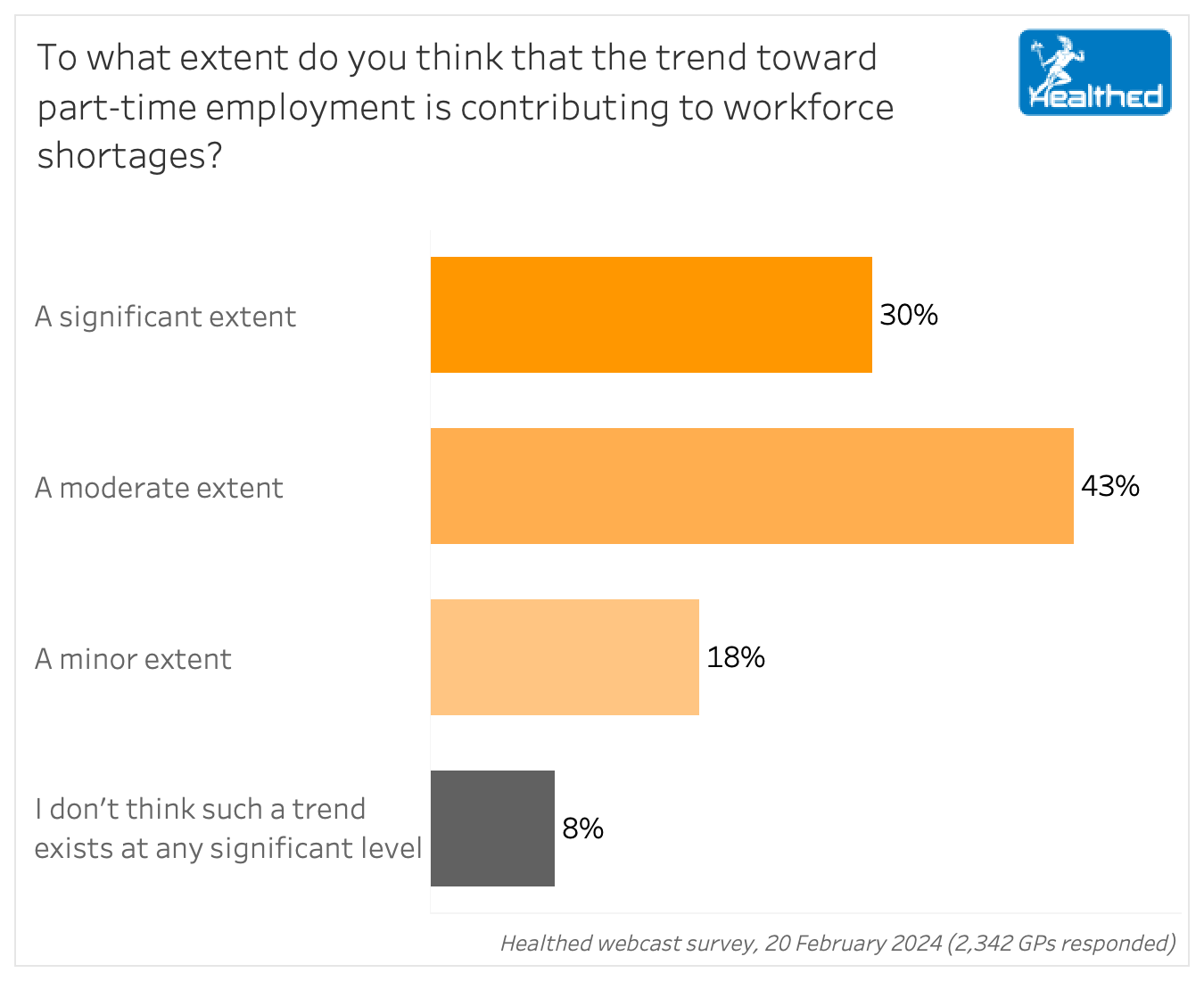
More than 70% of GPs in Healthed’s survey feel the trend towards part-time employment is noticeably contributing to workforce shortages.
The most recent Medical Deans Report found the proportion of medical graduates listing general practice as their top choice had hit a 10-year low at just 13.1%.
Eight out of 10 GPs in Healthed’s survey also said part-time work impacts continuity of care, with a new study by University of Cambridge researchers suggesting that disrupted continuity of care further compounds the workforce crisis.
Their analysis of data from over 10 million GP consultations in England showed that when patients saw their regular doctor, it was an average 18% longer before they needed to see a doctor again compared to patients who saw a different doctor—with no difference in the duration of that next appointment.
In free text comments from Healthed’s survey, several GPs said flexibility and better work-life balance may attract more people to general practice — and make it a more sustainable and satisfying option to retain them. Many also noted quality of care might improve as doctors would be healthier, happier and less burnt out.
Others pushed back on the notion that working part-time is a lifestyle choice at all.
“Part-time is not a ‘lifestyle’ option – it is a choice to maintain balance and sanity when the professional role/relationship with patients is ongoing and more demanding,” one surveyed GP said.
Another GP in her 30s who works part-time told Healthed that ‘times are changing’ and it’s not just medicine that’s experiencing the shift.
“This is what’s happening in other spheres of work too, so why should general practice be any different?” she asked.
“Insofar as younger doctors are choosing to avoid General Practice altogether,” one GP quipped in the free-text comments.
“It’s definitely not for the appreciation, respect or the money,” said another.
“Certainly the money and bureaucracy wouldn’t encourage them, only lifestyle is better than other medical pathways…,” another respondent observed.
Other GPs disputed that such a trend exists.
“More junior doctors want to be specialists as paid better and can work less – better work life balance,” one GP said.
“In my experience, those who start GP solely for the lifestyle quickly discover it is harder medicine than they believed and either leave or change their approach,” another noted.
“Not as much as in the past due to poor financial incentives compared to hospital specialists.”
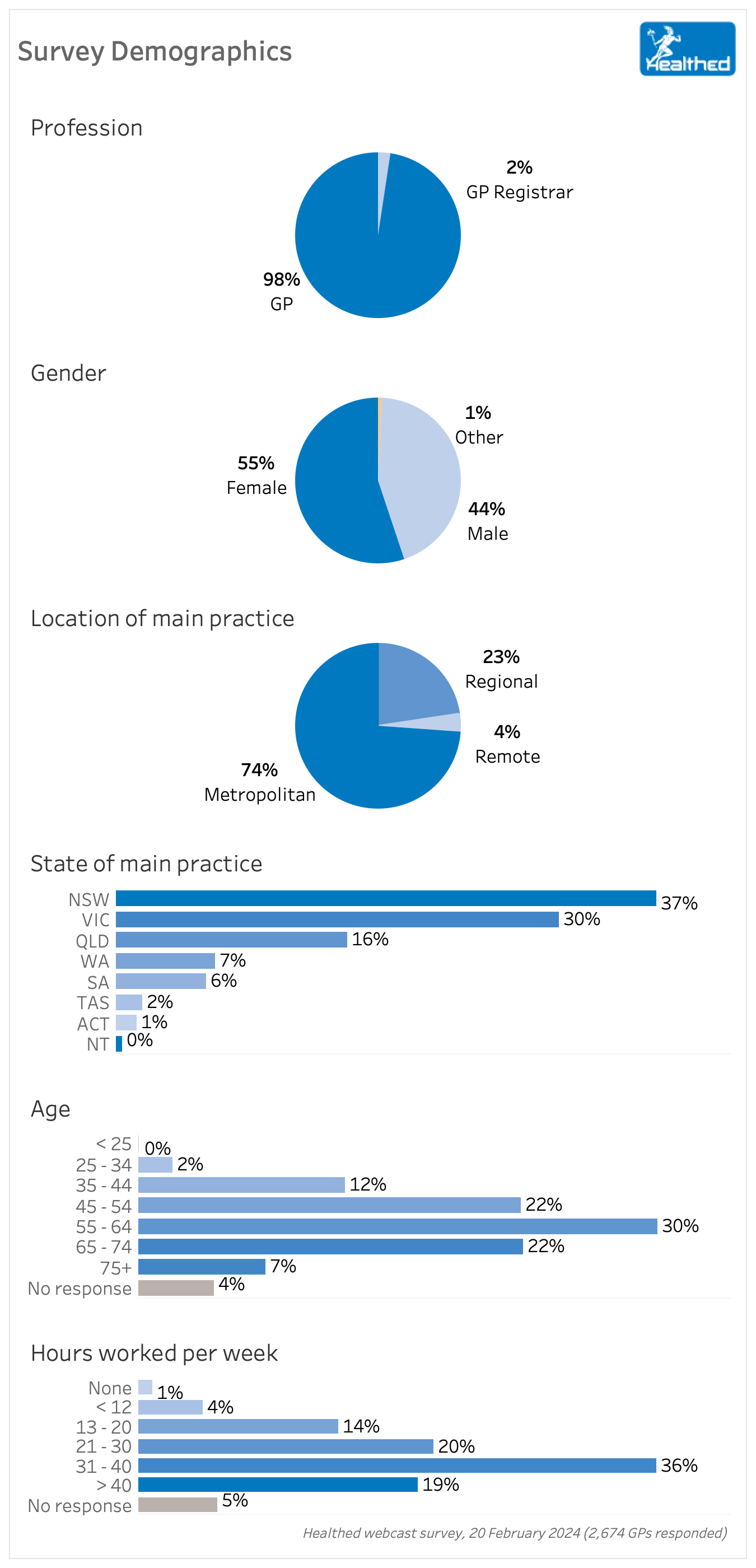
Survey conception and design – Dr Ramesh Manocha, Yasmin Clarke, Lynnette Hoffman
Survey analysis and visualisation – Yasmin Clarke
Writing and reporting – Lynnette Hoffman

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart


Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
