Articles / GLP-1 restrictions will make care trickier, but GPs supportive

As of 1 June, the government has placed new restrictions on several PBS-listed medicines for type 2 diabetes—with GLP-1 receptor agonists particularly targeted.
Nearly half of 1270 GPs who responded to Healthed’s survey Tuesday night expect the new restrictions to negatively impact management of their patients, while 20% predicted a positive impact, and 31% said there’d be no impact.
Despite this, 54% of GPs said they agree with the changes, while 46% disagree.
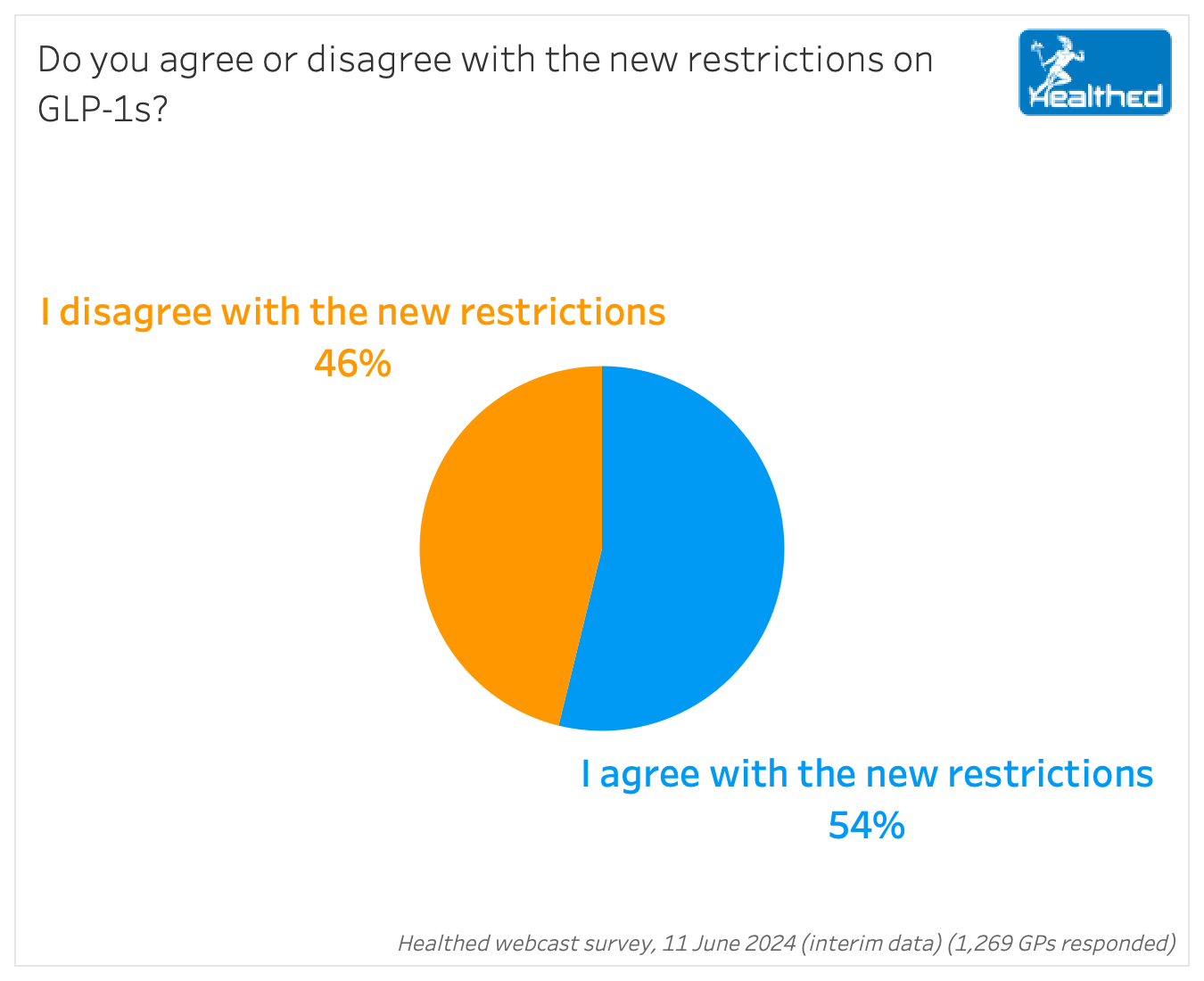
An online NewsGP poll last week found 59% of respondents did not support the PBS restrictions on GLP-1 RAs; 31% did support them, and 8% were unsure. While the numbers differ, both surveys show a considerable split between doctors – and highlight that many sympathise with the Government’s predicament.
Many GPs in Healthed’s survey believed the changes were prompted by drug shortages and access issues.
“Until supply is established, some method of rationing will be necessary,” one GP commented.
This is also how Diabetes Australia framed it as they announced the change to consumers, saying the “rules have been changed to ensure medicines like Ozempic and Trulicity are available for the people who need them most.”
Several GPs who supported the restrictions included the caveat that once supply issues were solved, the changes should be reversed.
“I agree with restricting while there is a shortage, but believe the benefit of these drugs long term would outweigh the cost once supply is available,” one GP explained.
However, in its extensive explanation, the Government never explicitly mentions supply issues and does not suggest the restrictions are temporary.
The Pharmaceutical Benefits Advisory Committee recommended the changes after an analysis of utilisation documented widespread use outside of the PBS restrictions.
The changes aim to simplify, clarify and improve adherence to PBS restrictions, and align with current clinical guidelines “while considering the cost-effectiveness of comparative treatment,” according to the rationale explained on the PBS website.
In 2021-22, GLP-1 RAs were the highest expenditure class of PBS-listed type 2 diabetes medicines—costing $194 million, and accounting for 26% of total spending on T2DM medication.
While many surveyed GPs felt the changes prioritised cost-savings to the detriment of patient outcomes, others felt it was a hard but necessary choice.
“They have a responsibility to manage funds, and if good control can be achieved with cheaper meds, it should be tried first,” one GP commented.
“There are limits to every budget. I consider that the government has a duty to spend taxpayers’ money as cost-effectively as possible,” said another.
Key changes include:
Notably, “the definition of a ‘clinically meaningful glycaemic response’ has been left open to prescriber discretion in the context of the individual patient.”
Counterintuitively, the government says the changes have “broadened access to GLP-1 RAs, by allowing use in patients that are not only contraindicated or intolerant to an alternative medicine (now SGLT2 inhibitors), but also those who do not achieve a clinically meaningful glycaemic response to an alternative medicine.”

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart


Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
