Articles / GPs predict instant test results nightmare

Despite warnings by several medical colleges, the Department of Health and Aged Care is forging ahead with its plan to eliminate the seven-day buffer and allow patients instant access to most diagnostic imaging and pathology reports shared to My Health Record.
While the Government claims this will empower patients and streamline clinical decision-making, 76% of GPs do not support the change, Healthed’s latest survey found.
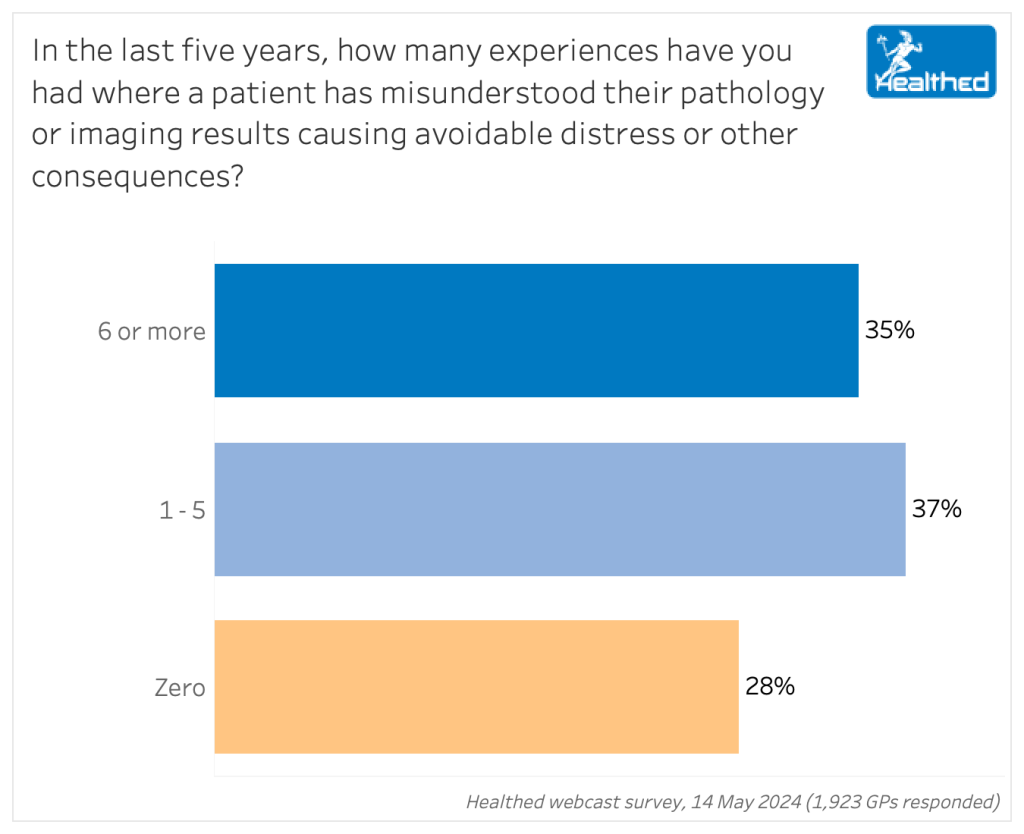
Seventy-two per cent of more than 1900 surveyed GPs reported first-hand experiences of their patients misunderstanding test results in the last five years, leading to needless distress or other consequences.
Eight out of 10 GPs are noticeably worried about the change, with 39% describing themselves as “extremely concerned” and 41% saying they are “moderately concerned.” Just 4% said they were “not at all worried,” while 16% were “slightly worried.”
Many GPs recounted the unpleasant realities of patients accessing their pathology or imaging without appropriate medical support — from cancer scares to confusion caused by positive herpes tests (and resulting relationship stress) — to a panicked patient who found out she was pregnant via a lumbar spinal MRI her physio had ordered, among countless others. Several doctors had patients who interpreted benign lesions as malignant, causing significant distress.
Approximately 40% of free text survey responses cited panic over normal or clinically insignificant finding as a key concern.
“A patient looked into his chest X-ray films and thought that he had a lung tumour/cancer, but actually it is just his heart,” one respondent wrote.
“Patient misunderstood the pathology results (minor impaired LFT due to an URTI/antibiotics) and told their family they have liver failure. Caused severe distress,” wrote another.
GPs were also concerned that:
Royal Australian and New Zealand College of Radiologists President Professor John Slavotinek said giving patients access to their report prior to consultation with their referring clinician could cause “significant anxiety and psychological harm.”
“Delaying the release gives doctors the opportunity to co-ordinate clinical decisions and care ahead of a patient receiving potentially life-altering news from a radiology report.”
It could also disrupt clinical workflows as “radiologists will have to spend more time reconsidering the language and content of the report for a non-clinical audience,” he said, noting the College has made their concerns clear to the Department of Health and Aged Care.
The Royal College of Pathologists of Australia also opposes the move, saying patients need support and guidance when interpreting complex diagnostic test results.
“Certain diagnostic tests, such as anatomical pathology and cytopathology reports, and genetic test results, contain medical jargon that often requires careful interpretation, and may have broader, more complex implications for patients. Immediate release of these results without appropriate context and interpretation could potentially lead to confusion and anxiety among patients,” they wrote in a press release calling for comprehensive consultation about the change.
But many surveyed GPs also feel patients should have the right to access their own information—even if they do have some concerns.
“It is not likely to be a frequent occurrence, but as results are in medical language it would be easy to misinterpret. On the other hand, I don’t feel patients should have to wait for more than 1-2 days to receive results that have already been reported,” one GP said.
Australian Doctors Federation Chair Dr Aniello Iannuzzi also holds nuanced views.
“Once upon a time medical records used to be the doctor’s own possession and that was about all there was to it, but the more modern approach is that they’re documents that are equally owned by the patient,” he said.
“It’s the patient’s information and at the end of the day the patient is really paying for it… even though with bulk billing the patient may not be putting their hands in their pocket,” he said.
Dr Iannuzzi hopes the change leads to less duplication and fewer requests for GPs to send results to specialists and hospitals.
“People tend to just expect GPs and their secretaries to provide this free information-sharing service. Hopefully giving patients results will reduce some of that burden on GPs, because that’s all work you do for nothing,” he said.
But he shares concerns about the potential misinterpretation of results, as well as incomplete or out of context results – and says the ambiguity could lead to medicolegal concerns.
The CEO of the Australian Patients Association (APA) David Clarke believes the change marks positive shift towards a more patient-centric approach.
The APA gets regular feedback from patients frustrated by lack of access to their information, he says, adding that not knowing your results can be unnerving.
“When the patient’s not properly informed, it creates unnecessary anxiety and stress and puts a whole other layer of concern over whatever their illness or condition may or may not be,” Clarke says.
“The impact of the stress that goes into people having to often wait for extended periods to get a next appointment with their GP, or for their GP to simply tell them some basic information that they could have probably gleaned themselves, is really unnecessary.”
Clarke says patients are smarter than they’re often given credit for, already turn to Dr Google to work out what their problem might be, and are likely to book an appointment quickly if they have concerns about their results.
The change puts greater onus on doctors to communicate well, he added.
“If there’s potentially a serious outcome to the diagnostic process, then the doctor needs to advise the patient about what the possible outcomes could be and reassure them that even if they are of a particular negative kind, that doesn’t automatically mean certain things,” he said.
Despite potential upsides, Dr Iannuzzi cautions the change could raise medicolegal issues for GPs:
“If the patient for example gets the result, does that release the burden from the ordering doctor at all in terms of actioning that? What are the rules of the game going to be with respect to the responsibility and the follow up? That’s the big unknown.”
Georgie Haysom, General Manager Advocacy, Education and Research at Avant, said giving patients immediate access to test results does come with risk if appropriate safeguards aren’t implemented.
“There is a significant risk of misinterpretation or misunderstanding when patients can access results without first discussing their clinical significance with their doctor,” she said. “This risk is heightened when patients can easily use the internet or AI tools in an attempt to understand results. This could lead to patients being unnecessarily distressed or even cancelling or ignoring follow-up arrangements.”
She says that regardless of when patients can access results, “it remains a doctor’s obligation to review results and contact their patients for follow up in an appropriate timeframe, depending on the clinical significance of the result.”
Doctors will also need to manage concerns and questions from patients that may seem out of proportion with the clinical significance of the results, she added.
“Doctors and their patients will benefit from clear communication about the process for contact after pathology results are available. Particular care may need to be taken with known vulnerable patients.”
Doctors should be clear on the steps to take when requesting that certain results not be automatically uploaded, Haysom said. For example, there may be a section to fill out on the request form.
“Importantly, any exceptions to the immediate upload of pathology results will need to be clearly articulated.”
The Government says diagnostic imaging and pathology providers should be uploading patient results to My Health Record by 30 June. Legal obligations to upload are expected to be in place by December this year.
Information from the Department of Health and Aged Care notes that while there will be some situations where healthcare providers can’t or won’t have to share diagnostic imaging or pathology results, “these will be the exception and not the rule.” You can find more detail about the change here.
What GPs are saying
“Perhaps the user unfriendliness of My Health Record will protect patients from access to information without their GP’s explanations or reassurance.”
“Most patients are intelligent and when they see the results, when they have questions, will seek clarification with their doctor if they trust the doctor. Seeing results beforehand enables patients to attend having thought through their results and have specific questions for their doctors to address. I think this is empowering the patients.”
“I support the rights of a patient to have access to their results, but they still need the guidance of a doctor to help them interpret/understand the results. Patients do not have the training to understand what the numbers mean or look at the overall picture. For example, they may worry about a red MCHC value outside the normal reference range while everything else is normal; yet they fail to grasp the nuance of a low normal Hb of 125 when it was 160 three months earlier (yet both numbers are within the normal range).”
“It’s fine for them to have, but some may disregard the results as being OK whereas the GP can see reasons to consult – and over-interpretation is not a good idea at all.”
“Chaos waiting to happen. You’ll see a lot of already stressed GP’s close their doors when patients hound them about every little red number that they try to interpret without medical training. Well done on another stupid decision.”

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart



Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
