Articles / GPs sceptical about RACGP’s triple bb incentive proposal

The RACGP is calling for the tripled bulk billing incentive to be extended to everyone under 35 – but GPs are not so sure.
In its pre-election pitch, the College argues this will prevent nearly 3,200 ED presentations and 9,200 hospitalisations, as well as improving preventative care, early diagnosis and chronic disease management, saving the health system and young Australians a combined $119 million each year.
However it comes at an estimated cost of $390.6 million to 557.8 million per year, depending on demand. That’s more than three times the expected savings, at a minimum.
And while it would no doubt benefit those who already bulk bill, it’s unclear how much the proposed expansion would meaningfully move the needle for mixed billing practices.
“It wouldn’t encourage me to bulk bill, but makes it more financially viable for the people I do bulk bill,” is how one GP in a national Healthed survey this week described the likely impact.
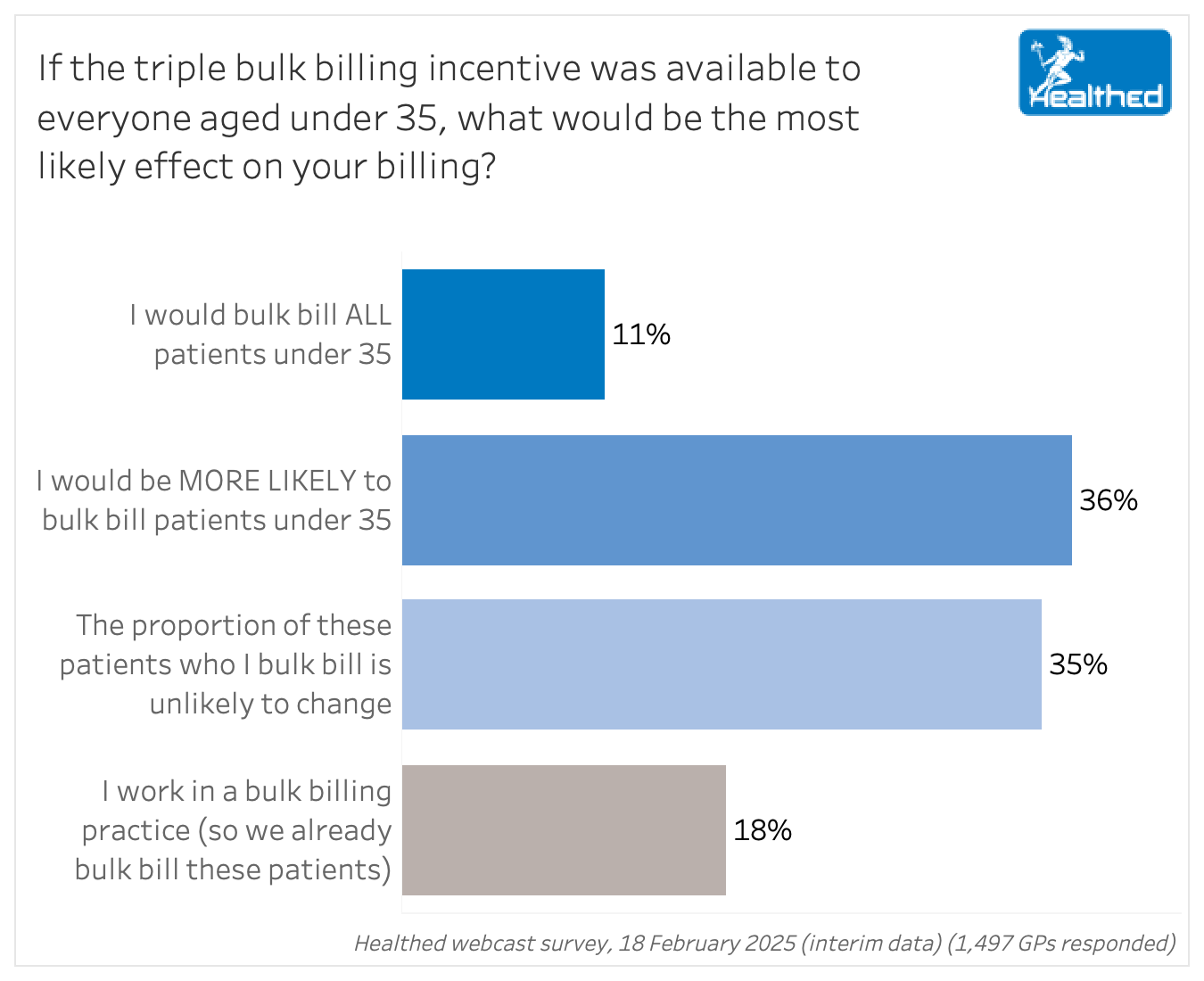
More than half of nearly 1500 GP respondents said expanding the tripled incentive would not change the proportion of patients who they bulk bill – while just 11% said they’d bulk bill all patients in the targeted age group.
“Medicare rebates remain low. I have completely ceased bulk billing so am unaffected, having shed my guilt & over developed sense of responsibility. Rebates need to be lifted globally, although I suspect the gap will continue to widen as practice viability threat grows,” another GP noted.
“For those patients I already bulk bill that would be most welcome. I may BB a few more people on occasion but not routinely.”
A further 36% of GP respondents would be “more likely” to bulk bill those aged 34 and under if the tripled incentive was extended to that group. For example, some said they might be more likely to consider bulk billing uni students or those experiencing hardship.
“I would restrict it to disadvantaged patients only – disadvantaged as judged by me, not Centrelink,” one GP explained.
“I might take into account income and chronic medical conditions requiring frequent appointments to guide the decision,” another GP said.
Overall, 41% of surveyed GPs support the proposal without caveats, while 39% like the idea in principle, but think the details need refining – and 20% don’t support it, full stop.
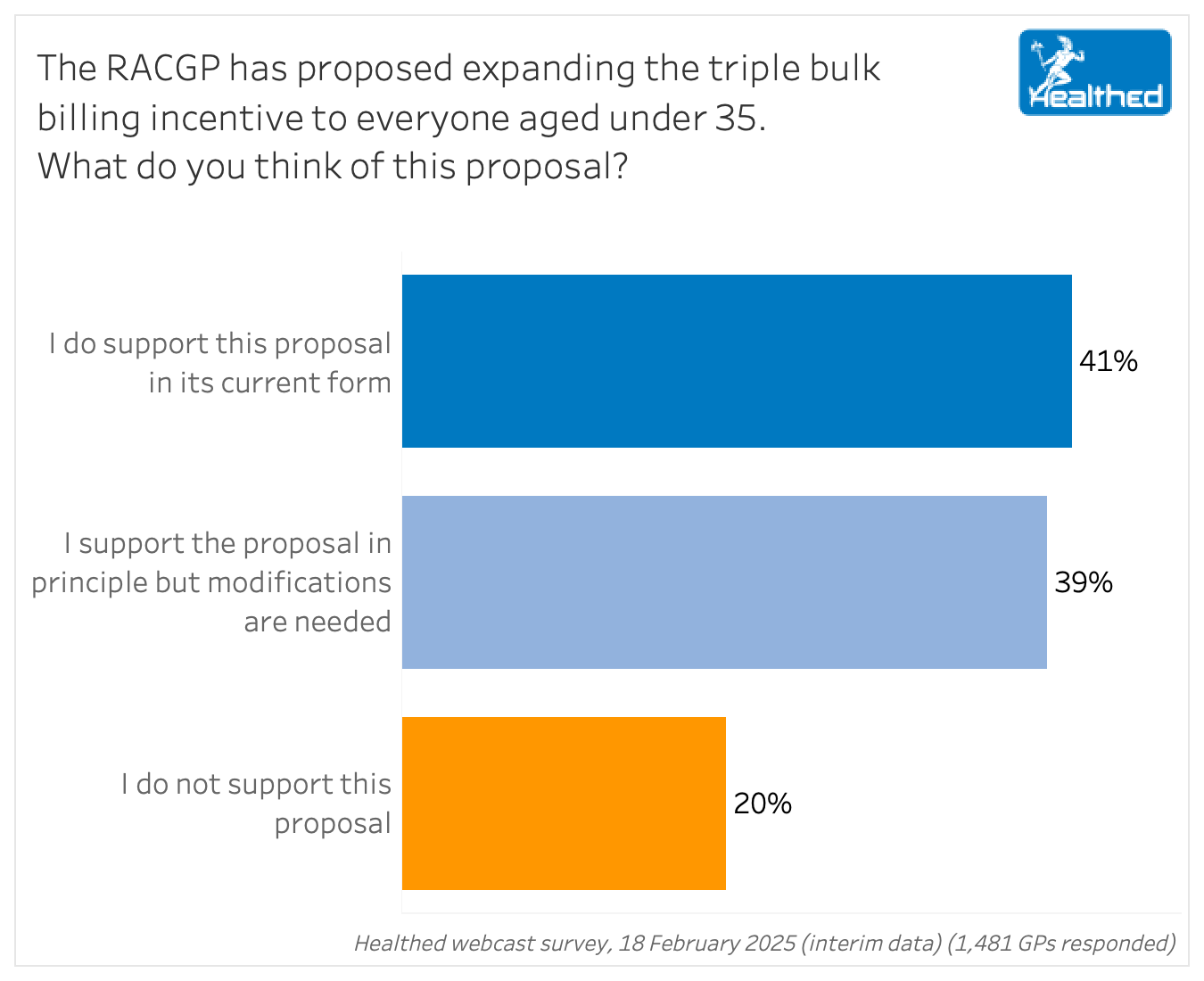
When we asked GPs to explain their choice, it became clear that those who said they support the proposal in principle – but with modifications – generally liked the idea of extending the tripled incentive to some additional patients, but questioned the equity and utility of the age-based cut-offs.
Many felt it should be means-tested, or focused on more vulnerable populations, such as the elderly, or those with chronic and complex conditions.
“I’m not sure that targeting under 35s will capture the most health needs,” one GP said.
“I don’t understand why the younger age group has been targeted,” another commented. “They are more likely to be well and less likely to have chronic illness. I think older people should get the triple BB incentive as they’re more likely to come to the doctor and have high healthcare costs.”
“Bulk billing should be for the disadvantaged and to ensure equal access to primary health care – it should not be available to those who have the resources to pay.” – surveyed GP
“There are many under 35s who regularly attend and have stable incomes – and a small gap is not problematic.”
“The incentive should be considered for patients under 25 and over 55-years – this is the most likely group of people that struggle with getting a regular job.”
“Bulk billing should be a privilege extended by doctors to those patients whom they know would benefit, irrespective of age.”
“This would certainly be of benefit to uni students, but I don’t think it should be offered to full-time workers.”
Others felt the incentive should either be applied universally to everyone.
“This should include every single patient regardless of their age. Tax payers need a financial help given the cost of living.”
Incentives not high enough to cover costs
Many GPs also noted that the bulk billing incentives are not adequate – and that the Medicare rebate should also be increased.
“The proposal is still not paying enough to GPs who bulk bill.”
“Higher government rebates are required. Current rebates are not sustainable for the cost of living.”
“I would still privately bill these people as the rebate is $30 short of what I charge privately.”
“Even tripling the BB incentive won’t get the patient rebate to an appropriate level, and this will put more expectation and pressure to bulk bill this group. But I do agree that people in this group need more support and probably have significant financial barriers to accessing care.”
“It still overlooks the fact that Medicare rebates have not increased in line with inflation generally and are still inadequate to support GP.”
By and large, GPs who support the proposal felt that people under 35 are often struggling financially, which can be a barrier to seeing a doctor and preventive care.
“Younger patients are usually more reluctant to see a doctor but with the tripled bulk billing incentive, it might encourage them to do so.”
“Every young person I have spoken to is struggling financially due to the cost-of-living crisis; some are putting off medical appointments – especially those who are in the low wage cohort.”
Others agreed, adding that they currently bulk bill these patients despite the toll it takes on their own hip pocket.
“The majority of my patients under 35 are not in a financial situation to prioritise medical care if there is a gap fee. I inevitably bulk bill them at my own discretion to the detriment of my mixed billing practice.”
“I end up bulk billing way too many people, especially if I’ve delivered them or have been treating them for the last forty years. Any improvement in the Medicare rate is welcome.”
What those opposed to the proposal are saying
But others said the tripled incentive was still insufficient to cover costs – and expanding eligibility would just pressure GPs to bulk bill at their own expense. Many felt the Medicare rebate should be the focus.
“It just means the pressure is on GPs to accept lower than appropriate rates. The Medicare item rebate should be increased dating back to following inflation over the last 25 years….”
“It will not adequately compensate to replace current private billing rates, therefore unsustainable to run a practice.”
“Practice costs, registration and indemnity insurance costs have gone up markedly during the Medicare item freeze and triple bulk billing incentive doesn’t even come close to the figure we need to keep practise viable.”
“I feel that the Medicare rebate should be increased to an acceptable level, not the incentive to bulk bill.”
“We should improve the standard rebates rather than the bulk billing rebates, the non-bulk billed patients are bearing the weight of the whole health care and they should be supported, rather than those who are bulk billed anyway.”
Others felt that broadly targeting young people was misguided.
“There are plenty of elderly people who are scraping by financially but not eligible for the bulk billing incentives and plenty of people carrying health care cards etc who are manipulating the system.”
“Most people under 35 have a job and can afford to pay for their occasional healthcare. Should not be an extra burden on the tax payer.”
“There are plenty of people aged under 35 who have the financial means to contribute to their health care. I had a patient this week age 30 who is buying a Lamborghini!”
Finally, several GPs noted that the proposal doesn’t address the root cause.
“Why is the RACGP focusing on bulk billing instead of ways to decrease GP burnout and improve sustainability of general practice? The RACGP has sold out to the government…”
“The triple incentive does very little to support growing general practice as a vocational choice for medical graduates. At best, it’s a band aid solution to address a chronic problem that has festered due to decades of neglect by state and federal governments.”

Postural Orthostatic Tachycardia Syndrome in Women

Panel Discussion on The Role of GLP-1 in the Management of CKD in T2D

Big Heads & Small Heads

Peanut Allergy



Increase
No change
Decrease
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
