Articles / How GPs can initiate treatment for eating disorders

Presentations of eating disorders skyrocketed during the pandemic, increasing the pressure on a health system that was already struggling to cope, with not enough specialists to address the need. This week ABC’s Four Corners highlighted the massive gaps in care and lengthy waiting lists that are leaving people with eating disorders and their families in a lurch. With patients sometimes waiting several months to see a psychologist or dietitian who specialises in eating disorders, GPs need to be prepared to help fill in the gaps in the interim. Eating disorder specialist Associate Professor Warren Ward says this three-step intervention can be started by GPs during that waiting period.
Re-nourishing both the brain and body is key to recovery
Brain starvation, the term for cognitive changes that people undergo when they restrict their eating, is a major cause of eating disorders—but it’s reversible with proper nourishment.
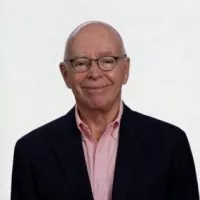
That fact underpins the best practice treatment approach of Warren Ward, Associate Professor of psychiatry at the University of Queensland, Director of the Ramsay Mental Health Eating Disorders Training Program, and co-author of the RANZCP clinical practice guidelines for eating disorders.
“If you’ve got two children and one goes on a diet, she’s 18 times more likely to develop anorexia,” says Associate Professor Ward.
The relationship between dieting and brain starvation was documented in a Minnesota study from the 1940s, where 36 men were given rations to lose 25% of their body weight.
“The men started thinking about food all of the time, they became depressed and suicidal, and they developed rules around everything, not just food. When they were re-nourished, they returned to normal again,” Associate Professor Ward says.
“I’ve seen this happen hundreds of times in so many healthy, normal kids and adults, where they starve their brains because of the culture around dieting, and all they think about is food and weight and they become very obsessive.”
Refer to a specialist, but don’t wait to treat
Psychological support is crucial to treatment, and if someone has indications of a disorder, they should be referred to a psychologist, psychiatrist or dietitian who specialises in eating disorders straight away.

However, given that it can take weeks or even months before a patient gets to see a specialist, Associate Professor Ward recommends that GPs start this three-step plan while waiting. The approach is considered the gold standard in treatment.
“When I started 20 years ago there were no evidence-based treatments that were effective. Now guidelines have been developed around a medical, nutritional and psychological stepwise approach,” he says.
The stepped plan is suitable for all types of eating disorders, and is successful in 75% of cases where the patient completes all three steps, according to Associate Professor Ward. It takes around 18 months to complete, and most studies report drop-out rates of about 30%, emphasising the need to educate patients about the health implications of brain starvation throughout the treatment.
In the first step, testing is undertaken to ensure the patient is not at risk of life-threatening cardiac complications. Associate Professor Ward recommends weekly testing for serum potassium, which can drop quickly if people are purging and vomiting, as well as phosphate, magnesium and glucose.
“Also test for postural hypotension and postural tachycardia. If the heart rate jumps up by more than 20 beats per minute, or the blood pressure drops by more than 20mm, that’s an indication for admission to hospital for supported re-feeding,” he says.
If a patient is barely eating, Associate Professor Ward recommends starting them on supplements three times a day, and to test their phosphate, potassium, magnesium and glucose levels weekly.
“A patient will never recover from anorexia on a normal diet. They need a high calorie diet to recover,” he says.
“Explain to the patient that by taking this nutrition they will avoid death, hospitalisation, and reverse the effects of starvation on their brain. Engaging family support can also be very helpful.”
“I get them started on high energy, low volume supplements like Sustagen, Resource, Fortisip or Ensure, which a dietitian can prescribe.”
Associate Professor Ward recommends tetra paks over powders, as powders give the patient the option to easily reduce their dose. Milk drinks, like Breakas and Up&Go, can also be effective.

“Three supplements a day is around 900 calories, which is enough to correct life-threatening cardiac complications, avoid hospitalisation, and start to reverse brain starvation,” he says.
“Ask the patient to try this for a few weeks to see if their brain becomes less obsessive and panicky around food and weight, and starts to function better.”
The next phase is to move the patient onto three meals and three snacks a day, with no more than three hours between eating, for a period of three months.
“It’s the rule of threes and the heart of the treatment. Ask the patient to see it as their heart and brain medicine, and a way to avoid falling into the OCD mode caused by inadequate brain nutrition. Regular nutrition also prevents bingeing,” Associate Professor Ward says.
The third step is an eating disorder treatment plan with a psychologist. Under the Medicare-supported plan, a patient with anorexia nervosa is eligible for 40 sessions with a psychologist, and a patient with bulimia nervosa or binge eating disorder can access 20 sessions. Dietitian appointments are also rebatable.
“There’s specific types of therapy, like CBT-E, MANTRA, FBT and SSCM, to help the person find other ways to deal with thoughts and feelings other than dieting and exercising,” Associate Professor Ward says.
For patients where the three step plan is not effective in an outpatient setting, GPs can suggest eating disorder units, day programs, and Australia’s first live-in residential program on the Sunshine Coast, Wandi Nerida.
In 2019, the federal government provided $63 million to develop their own residential treatment centres in six states and territories, but none have opened as yet.
A/Prof Warren Ward will be presenting at Healthed’s next webcast, regarding eating disorders and the role of the GP. You can register here for the next webcast held on Tuesday 7 March from 7pm AEDT.
Based on this educational activity, complete these learning modules to gain additional CPD.

Alcohol Addiction Assessment and Advice
Premature Ovarian Insufficiency – The New Guidelines

Paediatric Allergic Rhinitis & Immunotherapy

Inhaler Devices

Increase
No change
Decrease
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Webcast TONIGHT
POTS – What You Need to Know