Articles / The hidden cost of part-time GPs

Patients who see the same GP go significantly longer between consults than those who see a different GP in the same practice, a new UK-based study has found.
Researchers analysed data from more than 10 million consultations in 381 English general practices over an 11 year period, looking specifically at patients who had at least three consultations in the past two years.
Time to next consult was 18% longer for patients who saw their regular GP, with no difference in the duration of their next visit, compared with those who saw another GP.
“Importantly, if patients receiving care from their regular doctors have longer intervals between
consultations without requiring longer consultations, then continuity of care can potentially allow
physicians to expand their patient list without increasing their time commitment,” the authors wrote.
“The data show that the productivity benefit of care continuity is larger for older patients, patients with multiple chronic conditions, and patients with mental health conditions,” the University of Cambridge researchers explained.
They estimated that demand for consultations would drop by up to 5.2% if all practices matched the level of continuity attained by the top decile of practices.
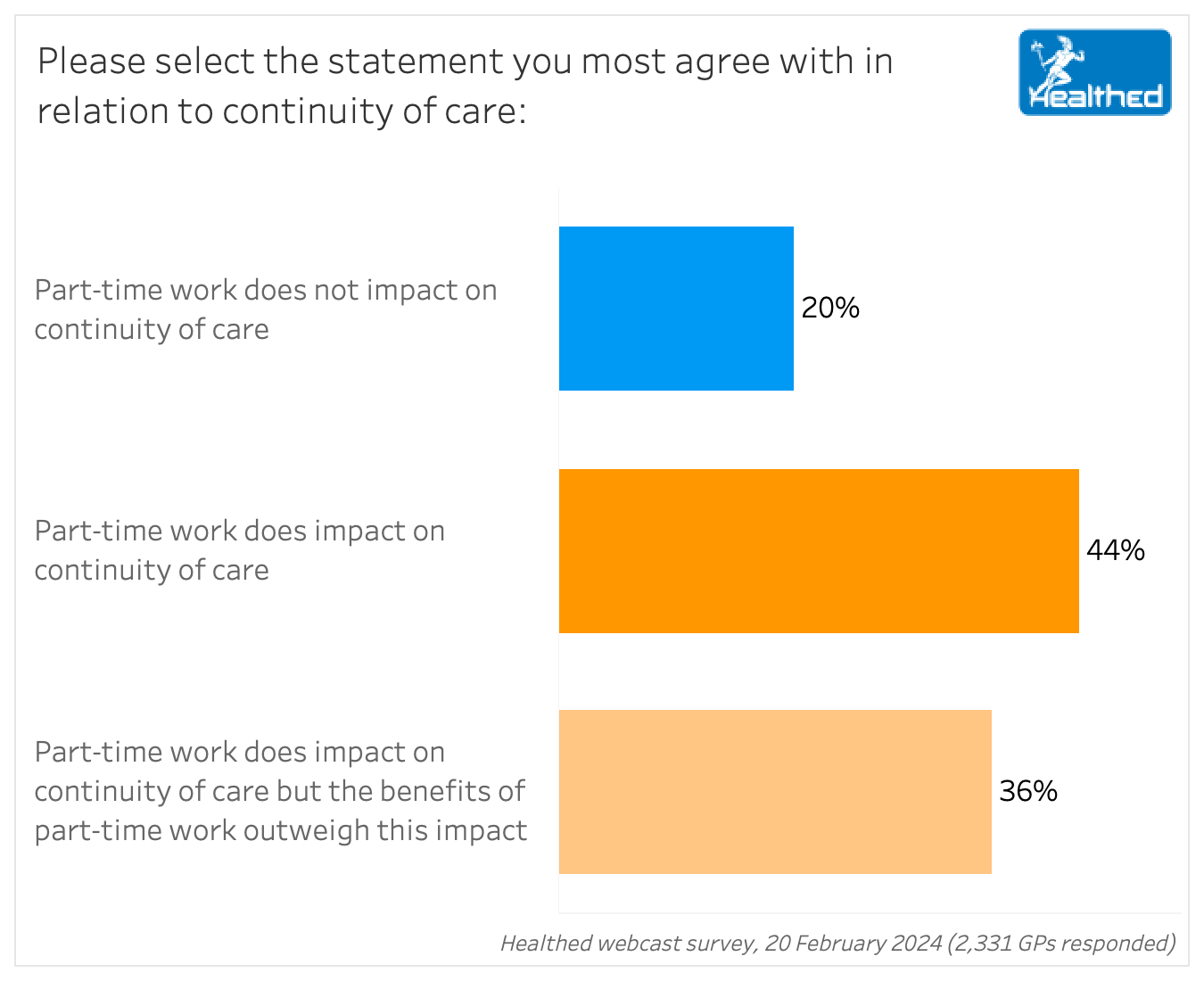
The RACGP’s annual Health of the Nation report has shown an increasing trend toward part-time work among GPs, and Healthed’s latest survey drilled into the potential impact of this, with 80% of GP respondents agreeing that part-time work affects continuity of care.
Despite this, 36% of these GPs felt the advantages of part-time work outweigh this impact.
In free text comments, many surveyed GPs said wins for work-life balance meant improved mental health and less burnout — with a positive flow on effect for patients.
“Greater job satisfaction means less burnout, leading to better patient care,” one GP said.
“Happy doctors, happy patients,” said another.
However, several GPs lamented that the shift toward general practice as a “lifestyle career” is negatively impacting continuity of care.
“Cradle to grave care will disappear as will daily continuity,” one GP wrote.
“It is getting harder to see your regular doctor for continuity of care. There are long waitlists, and often they are not taking new patients,” another GP summed up.
For more information: Manag Sci 2024; 24 Jan.

Alcohol Addiction Assessment and Advice

Premature Ovarian Insufficiency – The New Guidelines

Paediatric Allergic Rhinitis & Immunotherapy

Autism Spectrum Disorder – Managing Challenging Behaviours


Increase
No change
Decrease
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
