Articles / Scrap authority prescribing? Not so fast, GPs say…

More than half of GPs say the system has harms – overwhelmingly related to its time-consuming nature, with 62% saying it contributes to work stress and burnout, and 64% saying it significantly reduces available time for patient care.
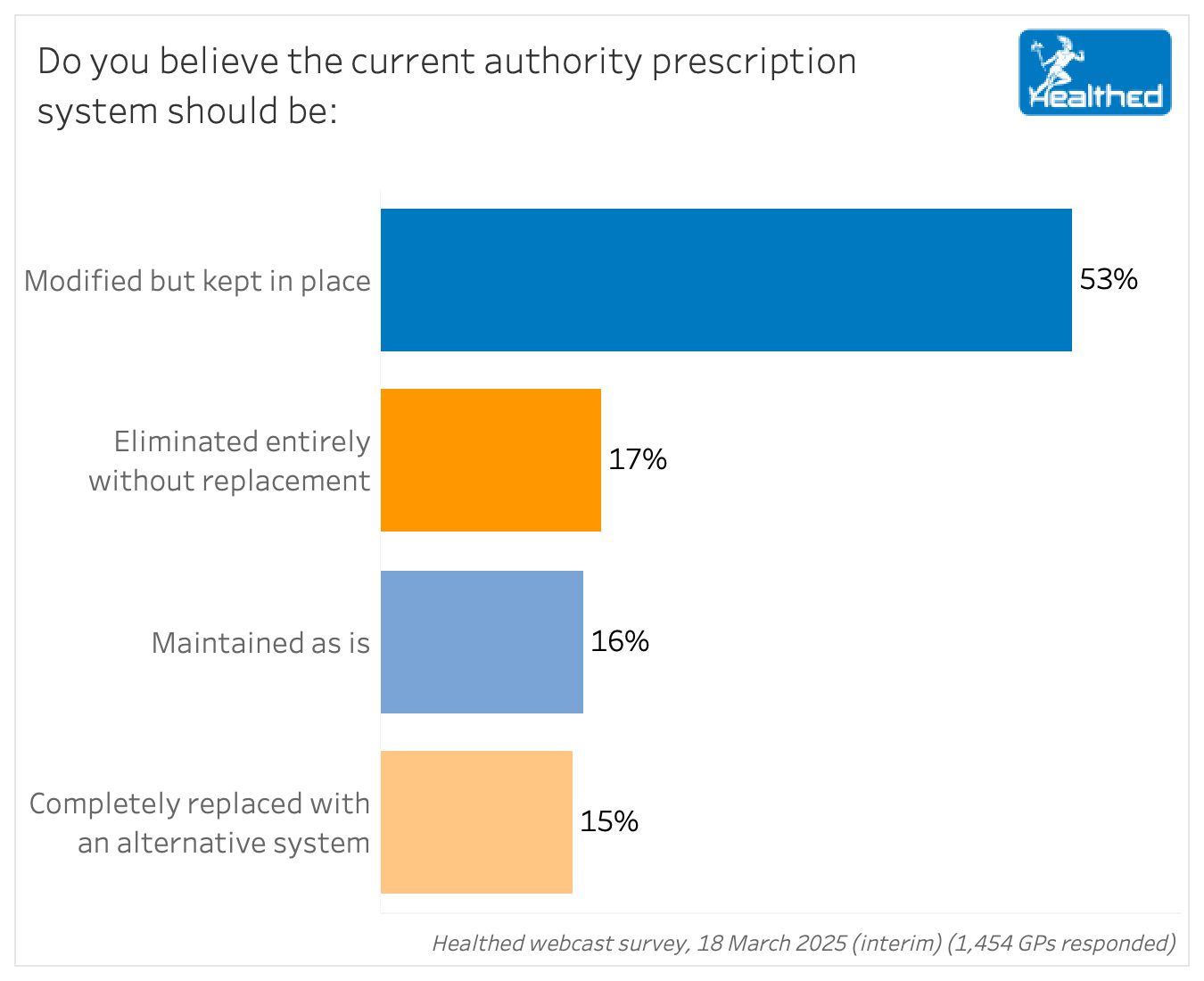
Which isn’t to say doctors think the system should be scrapped entirely.
Only 17% of doctors thought we should ditch authority prescribing without replacing it at all, while 15% said it should be completely replaced with an alternative system. The majority – 53% – said the system should be modified but kept in place.
The results come as an Australian National Audit Office report released late last year highlighted some troubling issues with the current system.
Three-quarters of Healthed’s survey respondents use the phone system rather than the online one. Surveyed GPs generally preferred phone due to ease of use, speed, and ability to multi-task, with many noting technical difficulties with the online system. “The online HPOS is hopeless – takes even longer than phoning,” commented one GP – a sentiment reflected by several doctors in the survey.
But the audit report showcased another concerning difference between the two modes: applications made by phone are more than twice as likely to be approved as those made online.
Specifically, the rejection rate for HPOS-based applications was 5.6% in 2023-24 — compared with a 2.3% rejection rate for phone-based applications.
The report also brought to light another issue: while the benchmark for Services Australia is to answer calls in less than 30 seconds, it has largely not met targets.
“Services Australia reports in its Annual Performance Statement on the achievement of a performance measure target of answering authority calls within 15 minutes. This does not align with the target of answering authority calls, on average, in less than 30 seconds,” the audit report stated.
So it’s no wonder GPs say the system is stress-inducing and causes “causes a significant waste of the doctor and patient time.”
In fact, three-quarters of the 550 GPs who commented on the harms the system causes cited the negative impact on both their and their patients’ time. Many described the annoyance involved, including “sometimes dealing with personnel who do not understand what they are talking about,” “longer consultations,” “time-pressure,” “stress,” and “hassle.”
However, despite the nuisance, most GPs felt some sort of safeguard was needed to ensure tax-payer money is used wisely and medications are safely and appropriately prescribed. “It’s good to have a system in place to prevent abusive use of taxpayer’s money,” is how one GP put it.
Clinical Associate Professor Pradeep Jayasuriya, a Perth-based GP with a keen interest in this issue, reckons the system needs to change with the times, however.
“The authority system has been around for a long, long time with some tinkering over the years, but the world has changed. The wider range of medicines and care is more complex, and really the system is probably not fit for purpose anymore,” he says.
In his view, the authority approvals process serves two purposes.
“One objective is obviously to ensure that prescribing is compliant with PBS requirements and the other is as a cost saving measure,” Associate Professor Jayasuriya says.
“Now, interestingly, as far as I know, those aims have never been rigorously evaluated. I haven’t seen a publication recently around the effectiveness of the authority system—how much it saves money and how much has it improved prescribing.”
He argues there’s more to quality use of medicine than ensuring prescribers meet the PBS requirements.
“Unfortunately, the government has walked away from quality use of medicine initiatives,” Associate Professor Jayasuriya says.
“This is perhaps the only remaining policy lever that they’ve got, given that they have defunded the NPS, which is probably the most effective quality use of medicine program that we’ve ever had.”
Additionally, he says the administrative burden and time-factor should not be underestimated.
“The Government is saying elsewhere that they recognise that GPs are now overworked, and there are serious access issues for patients. So on the one hand, they’re trying to increase that prescriber workforce. But on the other hand, they have done nothing about the red tape that GPs have to face, which then acts as a barrier to prescribing medications to patients,” he says.
While specialists also find the system frustrating, they have a smaller group of drugs to be across than GPs do, Associate Professor Jayasuriya notes.
“And some of the newer drugs have quite complicated PBS requirements. I think some simplification of that is necessary,” he says, adding that mistakes occur due to the complexities of those requirements.
Around 300 GPs in the survey provided specific suggestions for what modifications are needed.
The most common suggestion involved a simpler, more streamlined, automated process with better integration into prescribing software – followed by tweaks to improve the existing systems, such as hiring more staff to answer the phone and making online access easier. More than a third of respondents (35%) specifically mentioned streamlined processes, and even more alluded to it.
Currently 29% of medicines are authority-required – and about 14% of GPs said it should be far fewer, with several suggesting it should be restricted to Schedule 8 drugs.
“Take most drugs off authority, and simplify the process by not having so many different codes for the same dose, quantity and repeats,” one GP summed up.
“Modified streamlined system where GP confirms patient meets ALL the authority requirements.”
“Make the authorities all streamlined – you still have the list of approved indications, but without the waste of time.”
“Incorporate into practice software rather than having it as a standalone thing.”
“Streamlining and simplification of the guidelines and formatting of the software to make the criteria easier to follow. Currently is a convoluted nightmare for many drugs.”
“Easy to follow checklists of necessary PBS indications.”
“Have a computer programme that is integrated with practice software so you don’t have to work between two programmes that don’t communicate with each other, it creates extra work and stress.”
“Maintain sufficient staff at the end of the phone line so that the phone will be answered by a human being within 2 minutes at most.”
“More staff to answer a bit faster would help.”
“Make ONLINE access easy and simple.”
“Make it user and time friendly.”
“Consider an auditing process for prescribers, rather than authority scripts.”
“We should be trusted to do what is required. They can easily monitor use anyway and send letters out, like they already do, to let doctors know if they are doing the wrong thing.”
“Each ‘authority’ script should have clear eligibility, which we link to the patient’s history. Random audits can pick up doctors who are prescribing outside criteria.”
“A better My Health Record which would automatically check for Authority eligibility. An AI version?”
“Streamline automated processes.”
“Restrict it to drugs with a high risk of causing harm to patients, such as S8.”
“Eliminate many drugs on it – e.g., Nexium. Eliminate having to call for increased quantities.”
“It should be used for highly specialised medicines i.e. medicines that are commenced in hospitals or by specialists.”
“I don’t think we need anything like this except for massively expensive drugs like cancer drugs, some of the immune therapy for rheumatology, dermatology etc.”
“Just monitor controlled drugs.”
“Some authority medications such as PPI rescripts should be scrapped altogether, other medications such as S8 drugs and ones that are costly should be kept, but there should be a more effective way to gain access than the current system. We should not be kept waiting for someone to pick up the phone!”
Thanks to GPs Clinical Associate Professor Pradeep Jayasuriya and Clinical Associate Professor Marita Long, for their assistance with developing the survey questions.

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart



Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
