Articles / Losing WIP and PIP, a major negative for general practice – national poll

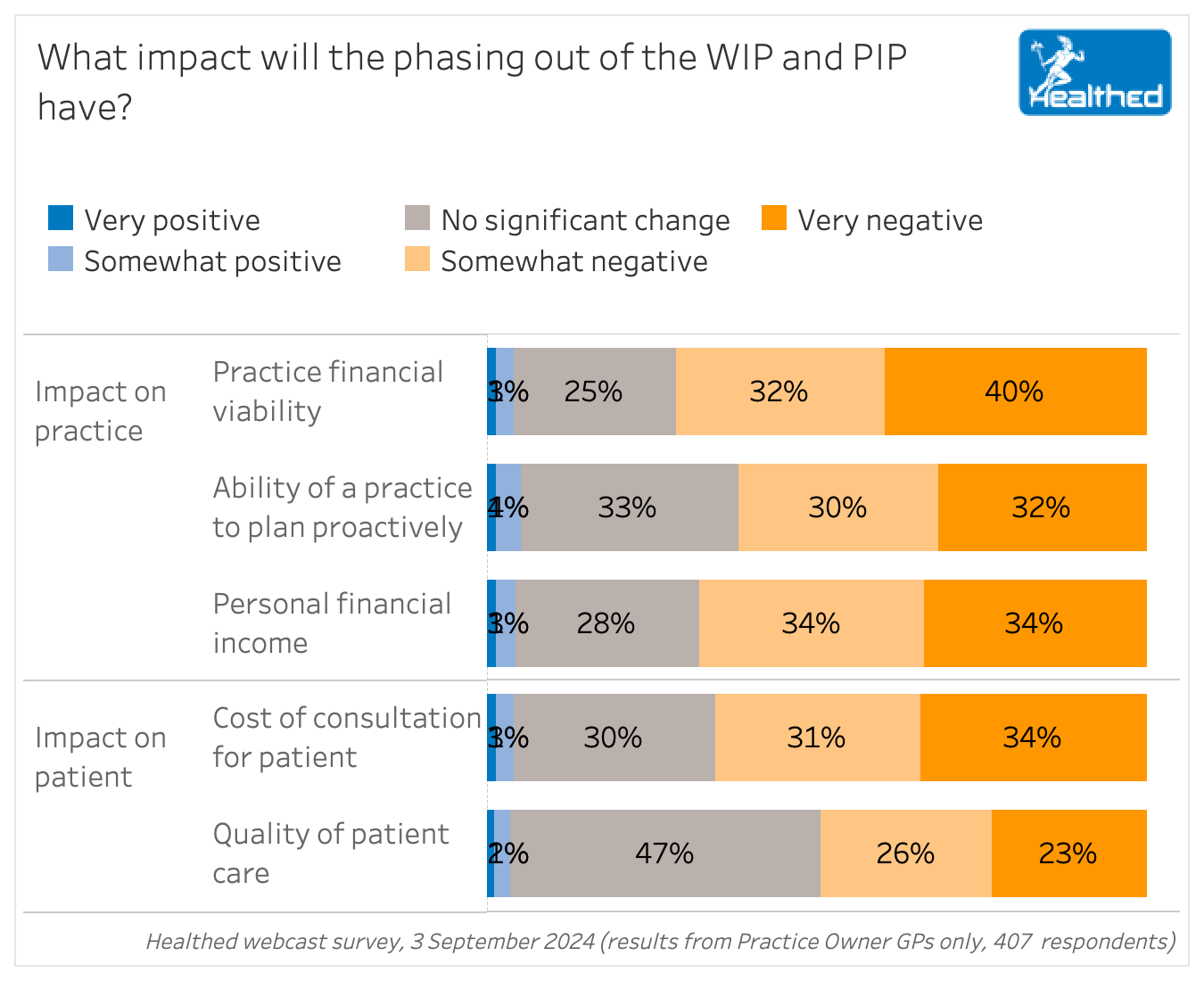
Around three quarters of GPs say losing WIP and PIP will negatively impact the financial viability of their practice – with 40% of practice owners predicting a “very negative” impact, according to a Healthed survey of more than 1500, which included 407 practice owners.
Yet an expert panel evaluating general practice incentives recommended phasing out the Practice Incentives Programs (PIP) and Workforce Incentive Program (WIP) Payments, describing them as “not actually essential for the survival of private practices” at a recent webinar.
GPs in Healthed’s survey were overwhelmingly concerned about the plan.
Key findings:
“Without the WIP we will not be able to afford to hire a nurse and without the PIP the surgery will definitely not survive, we are only a bulk billing practice, our patients cannot afford to pay for consultations,” one GP explained.
A nine-person expert panel, which included two GPs, recommended “a new, simplified general practice payment architecture” that aims to eventually replace WIP and PIP.
However, what exactly that would entail remains quite vague, though some details were telling.
The panel wrote that the payment architecture should “require general practices and patients to participate in MyMedicare,” for example.
It should also require practices “to provide comprehensive service delivery information, and data to support calculation of reimbursements, planning, evaluation, monitoring of health outcomes and quality improvement,” the panel recommended.
Primary care payments would increase from 10-40% “at the system level” by 2032, leading to “stronger multidisciplinary teams” as patients will be seen by the most clinically appropriate health professionals working at the top of their scope.”
In the meantime, the panel recommended that all current WIP payments be directed to general practices, rather than individual health professionals, “to enable flexibility and agility in attracting, recruiting and retaining health workforce professionals into rural and remote practice.”
Like 91% of GPs in Healthed’s survey, Australian GP Alliance deputy chair and past president of the AMA Dr Mukesh Haikerwal sees the phasing out of PIP and WIP as a negative for general practice, suggesting they are part of a larger trend of hypocritical policies that undermine GP.
“It beggars belief that you have a government or a minister who purport that their biggest concern is general practice and its longevity, yet they’ve done nothing to support it and everything they can to destroy it.”
“Current system works well now… Many patients are unable to get onto my Medicare [language, age, etc.] and it is an unnecessary burden, especially for those in nursing home, the provisions are very proscriptive.” – Surveyed GP
“I have no reason to believe (based on my years of life experience in general practice to date) that the WIP and PIP income will be adequately replaced by some other means in a straightforward fashion,” one GP commented.
Others predicted it would de-incentivise preventative medicine, discourage practice ownership, and drive consultation costs up.
“Taking away one of very few incentives to assist in keeping general practices afloat will be a negative impact. The profit margins are getting smaller every year, and this is yet another assault on GP as a business.”
Around one in 10 surveyed GPs agreed with the recommendation to replace PIP and WIP: “It is an unrealistic payment process, manipulated by everyone,” one GP said. “I don’t know yet…but it seems the money could be better spent elsewhere,” reflected another.
Others said if the change goes through, it will lead them to increased consultation costs.
“I think practices will use this as an excuse to start private billing. Once this has begun, I have not seen a practice reverse the decision to privately bill even when Medicare re-imbursements are increased,” one GP commented.
“It will reduce the number of people I bulk bill,” another GP said.
“We will have to look for other ways to make up the income and this may have financial implications for patients,” another agreed.

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart


Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
