Articles / Most GPs support assessing older Drs – national survey

While many prominent GPs have been outspoken in their opposition to the mandatory checks proposed by the Medical Board for late career doctors, Healthed’s national survey shows most GPs support assessments, particularly if they’re done by their peers, rather than by occupational specialists.
So far 2287 GPs have responded to Healthed’s survey about the Medical Board’s proposed solutions to the disproportionate number of complaints levelled against doctors aged 70 or older — with 59% in favour of assessments.
Half agree with the Board that a general health check with a GP is the most appropriate response, while 9% support extensive assessments by a specialist occupational physician. But 41% feel nothing extra needs to be done to ensure safe care.
While the consultation period on assessments for late career doctors is still underway, the Medical Board has outlined their proposal in great detail in a “consultation regulation impact statement” that you can download from their website.
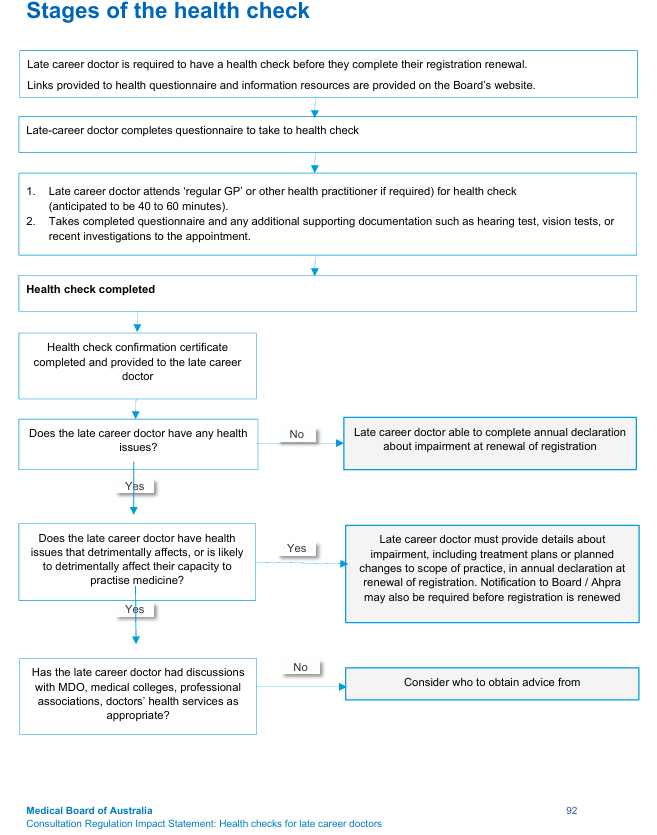
From age 70, doctors would be required to undergo general health checks with their GP or another doctor every three years, with the frequency of assessments increasing to yearly from age 80 onwards.
“In most instances, the checks would be conducted by the late career doctor’s regular GP, with some components of the health check able to be performed by other health practitioners with relevant expertise, such as audiologists, optometrists, or nursing staff in the general practice,” the Board explains.
The Board emphasises that results would remain confidential between the late career doctor and their assessing/treating doctor.
“The Board would NOT receive information about any health issues identified in the checks and would NOT receive any results of the health check.”
However, doctors would have to self-declare any impairments that could affect their capacity to practice medicine on their annual registration renewal form.
The proposed health check would take between 40-60 minutes, plus about 10 minutes to fill out the questionnaire, and would cover cognitive function, as well as cardiovascular, respiratory, gastro-intestinal, genito-urinary, mental health, neurological, musculoskeletal, manual dexterity, skin and heamatology, hearing, endocrinology and sight.
The appendix of the consultation even includes a draft algorithm, questionnaire and sample assessment form, suggesting the proposed mandatory health checks may be more than a theoretical debate.
Healthed survey shows a clear divide between older and younger GPs when it comes to support for the proposal. For example, half of GPs aged over 60 want to maintain the status quo, while just 30% of GPs under 60 think that is the best response.

Like the Medical Board, GPs in the survey preferred the option where the checks are done by a GP, rather than an occupational physician. Even GPs who aren’t keen on assessments overall much prefer peer-led health checks over specialist-led assessments.
When we asked how strongly GPs agreed or disagreed with the proposal to require mandatory health checks by their peers, 47% agreed, 20% were neutral and 33% disagreed.

While there were fewer GPs in the oldest and youngest cohorts, they had the most polarised views. GPs aged 35-54 were much more likely to agree with GP-led mandatory health checks for doctors aged 70 and up, while doctors aged 65 and over were more likely to disagree with them than their younger colleagues.
Despite 59% of surveyed GPs supporting mandatory assessments, a number of prominent doctors are unconvinced.
Dr Mukesh Haikerwal, a Melbourne GP, chair of Australian GP Alliance and past AMA president said the proposed assessments are “another insidious step by the regulator.”
“What makes it worse is the risk for the GPs who do the reviews and therefore take responsibility for whatever the diagnosis is, and can be subject to some kind of legal challenge for writing somebody off for some reason,” Dr Haikerwal said.
He also questioned the effectiveness of the proposed plan, noting that Queensland and New South Wales mandate driving tests for those aged 75, while Victoria does not—yet there’s no difference in rates of problem drivers between those states, he said. “So it shows that there is actually no rhyme or reason for what’s being suggested as a broad-based slap in the face of practitioners.”
Professor Karen Price, immediate past president of the RACGP, GP and researcher, also opposes making the checks mandatory.
“In my research and experience it seems the nudges to perform self-care are more likely to be enacted when a well-known peer nudges you firmly, than an unknown assailant from the health department,” she told Healthed.
Dr Aniello Iannuzzi, a GP and chair of the Australian Doctors Federation, said the figures from the Medical Board lacked detail and “should not be relied on to justify or legitimise a drastic escalation of regulation.”
“It strikes me as an emotional headline triggering a very heavy-handed response,” he added.
“Making health checks compulsory will ensure older GPs look after themselves, seek out a GP for their own health and yes, get confirmation in that they are still well and fit to continue practising as a doctor.”
“I am older myself and acutely aware of my cognitive processing speed being slower now, especially when fatigued. I thus do not see myself as agist. I have had concerns about older colleagues in the past, which have been happily resolved. I do think it is sometimes hard for older doctors to recognise their limitations…so I do think measures need to be put in place.”
“All doctors should have health checks at some stage because doctors don’t have GPs.”
“Thats ageism – we should have health checks for all doctors every two years, regardless of age.”
“Disagree with AHPRA stepping in again to regulate this age group. We, as the actual professionals should care for our grandparents of medicine. They should be able to hand on their arts of medicine without being scrutinised by the police body, AHPRA.”
“In practice it could/should be done with a GP, but it places a very high level of medicolegal expectation/risk on GPs. A specialist ‘GP assessment clinic’ with adequate time/resources might work.”

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart


Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
