Articles / Path companies make millions from repeat tests

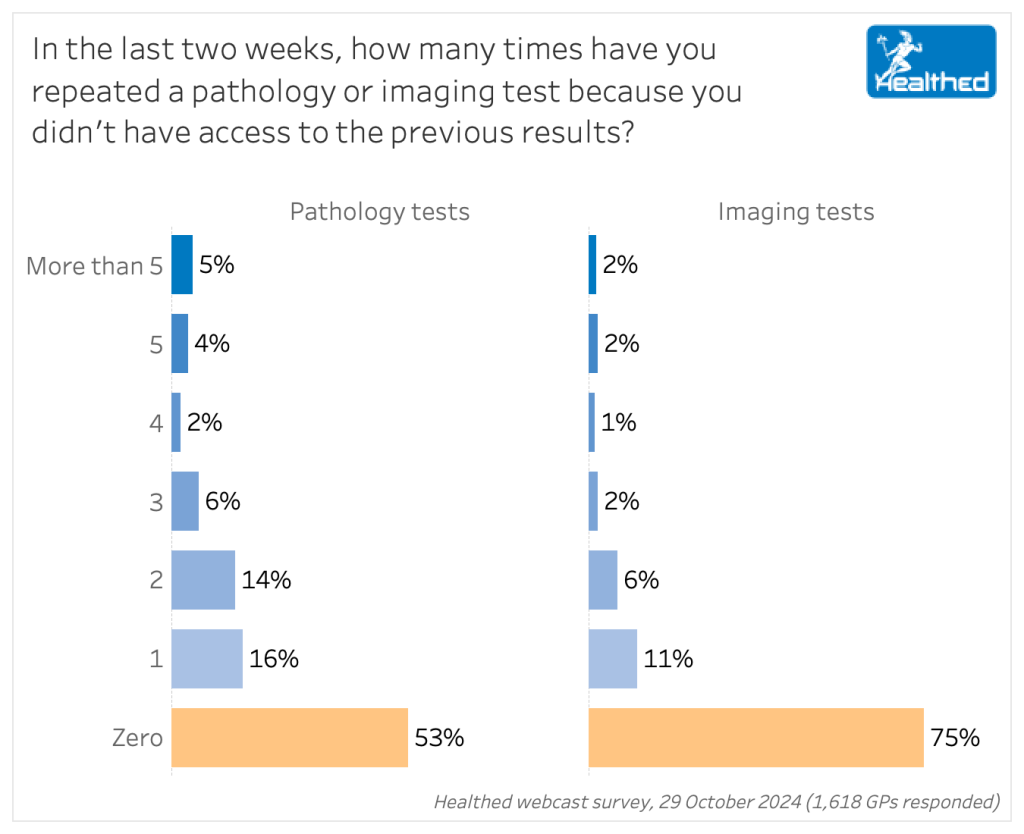
Inaccessible pathology and diagnostic imaging results forced 50% of GPs to repeat tests and scans in the past two weeks, according to Healthed’s most recent survey of over 1600 GPs.
At least 2,103 potentially unnecessary pathology tests were ordered by this cohort of GPs in a two-week period in October because they did not have access to previous results. Extrapolating that out to an estimated 23,000 GPs nationally, that means approximately 30,000 pathology tests were repeated in a fortnight because the GP was unable to access the initial results.
Likewise the survey showed that at least 965 scans were repeated due to inability to access earlier results – which works out to about 13,000 imaging tests nationally.
The financial incentives for pathology and diagnostic imaging companies to maintain these inefficiencies are immense.
So it’s no wonder that 65% of GPs think favourably of Health Minister Mark Butler’s recently announced plans to mandate pathology and diagnostic imaging companies to upload results to My Health Record – or lose out on the corresponding MBS payments if they don’t.
But — and it’s a big but — two thirds of those who support withholding payments when results aren’t uploaded said the Government needs to fix My Health Record first.
Wastage in the health system is a massive problem, says Dr Ollie Waters is a WA-based gastroenterologist who has built a searchable atomic pathology database, MyPathology, that allows you to access all pathology results from 2005 onwards, to help reduce the repeated tests.
He points out that pathology is approximately $5 billion a year business – with 80 million tests done in the community in 2020 alone.
“And we know that up to 40% of these tests are unnecessary or even potentially harmful,” he adds.
Like so many GPs in the survey, he supports the Government’s proposal in principle, but says it does not adequately address the “well documented problems” with My Health Record – its poor user experience. He says pathology companies have no impetus to change that, and in fact are partly responsible for it, as they insisted that results be uploaded as PDFs when My Health Record was being designed in 2014.
“Pathology companies are essentially data companies – and they have been putting barriers in place to limit clinician access to that data for many years which has resulted in higher profits,” Dr Waters says.
“I think this is a great proposal that the government should pay for the data, not the test, as the test is essentially meaningless unless the data can be accessed.”
He also dismisses the notion that requiring companies to upload the results will significantly increase costs, noting that it’s “the digital equivalent of adding a Cc to an email.”
It’s no secret that My Health Record is “clunky,” “cumbersome,” “time-consuming,” and a “nightmare to navigate” – to borrow some of the descriptors GPs used in a recent survey where 70% said it was failing.
Dr Waters argues that patient privacy concerns, poor searchability and user experience (UX) and more than a decade of missing data are all key issues that need to be solved to make a significant dent in the number of avoidable repeated tests.
“Approximately 10% of patients have opted out of My Health record, mostly for privacy reasons, so this will not help those patients,” Dr Waters says.
“We need a system with more flexibility that can capture data when a patient needs it, for example when admitted to hospital, and then can be deleted when the patient does not need it.”
Another problem is the huge backlog of results from the last 10 or 15 years past that have not been uploaded, he says.
“This is all highly relevant data for many patients’ health needs and there is no capacity to access billions of dollars worth of data through My Health Record.”
“The user experience of the system is woeful,” Dr Waters adds. “There is no point having the data there if it cannot be searched, or graphed over time, especially when managing patients with chronic diseases.”
“It’s got to be intuitive to use… Bearing in mind GPs have six minutes per standard consultation. So if you ask a GP to log into a system that takes two of my minutes, they’ve wasted 33% of their consultation time trying to find data, hence GPs and other doctors rarely use access MyHR.”
“So, to put that in the context, the Australian Digital Health Agency, the system owner of My Health Record are focused on digital infrastructure at the moment, and they’re not focused on UX. And that’s the problem.”
On the upside, Dr Waters says the Australian Digital Health Agency sponsored a trial of his MyPathology app which showed many positive clinical outcomes – a proof of concept.
“In 2019 we did a trial in a hospital outpatient clinic, two specialist rooms, and in a GP practice.”
“After the six months, surprise, surprise. We get better health care if doctors have better access to data.”
Doctors were more confident about diagnoses, started patients on treatment sooner, discharged more patients and ordered less blood tests.
“The pathology costs in the clinic came down by 66%,” Dr Waters says. “You can understand why pathology companies want to make data less accessible…”
“I think concerns for patient’s confidentiality is something that may be overlooked in this process, but overall I think it would improve patient care and reduce costs.”
“I chase all pathology and radiology results at my expense for the patient”
“Constant frustration that I can’t get previous results, especially from hospitals; patients can’t recall or don’t know which provider was used; they want a “second opinion” and want me to do all the tests again ‘to be sure.’”
“It’s a no brainer that accessing patient results instead of repeating the same tests over and over again will reduce healthcare cost and improve patient outcomes with more continuity of care. It is a double-edged sword, as this comes with increased risks around confidentiality breaches.”
“In my experience it is almost always possible to get hold of results with a little effort.”
“It would save so much time for me, and would save the patient time and an appointment if results were available at consultation.”
“Results can be obtained if need be – results do not have to be centralised.”
“The concerns regarding hacking of information remains paramount as it is no longer a theoretical risk.”
Survey demographics were 51% female, 48% male with 69% practicing in metropolitan areas, 26% in regional and 5% in remote areas. The median age bracket was 55-59.

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart



Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
