Articles / Racism a common experience for IMGs – Survey

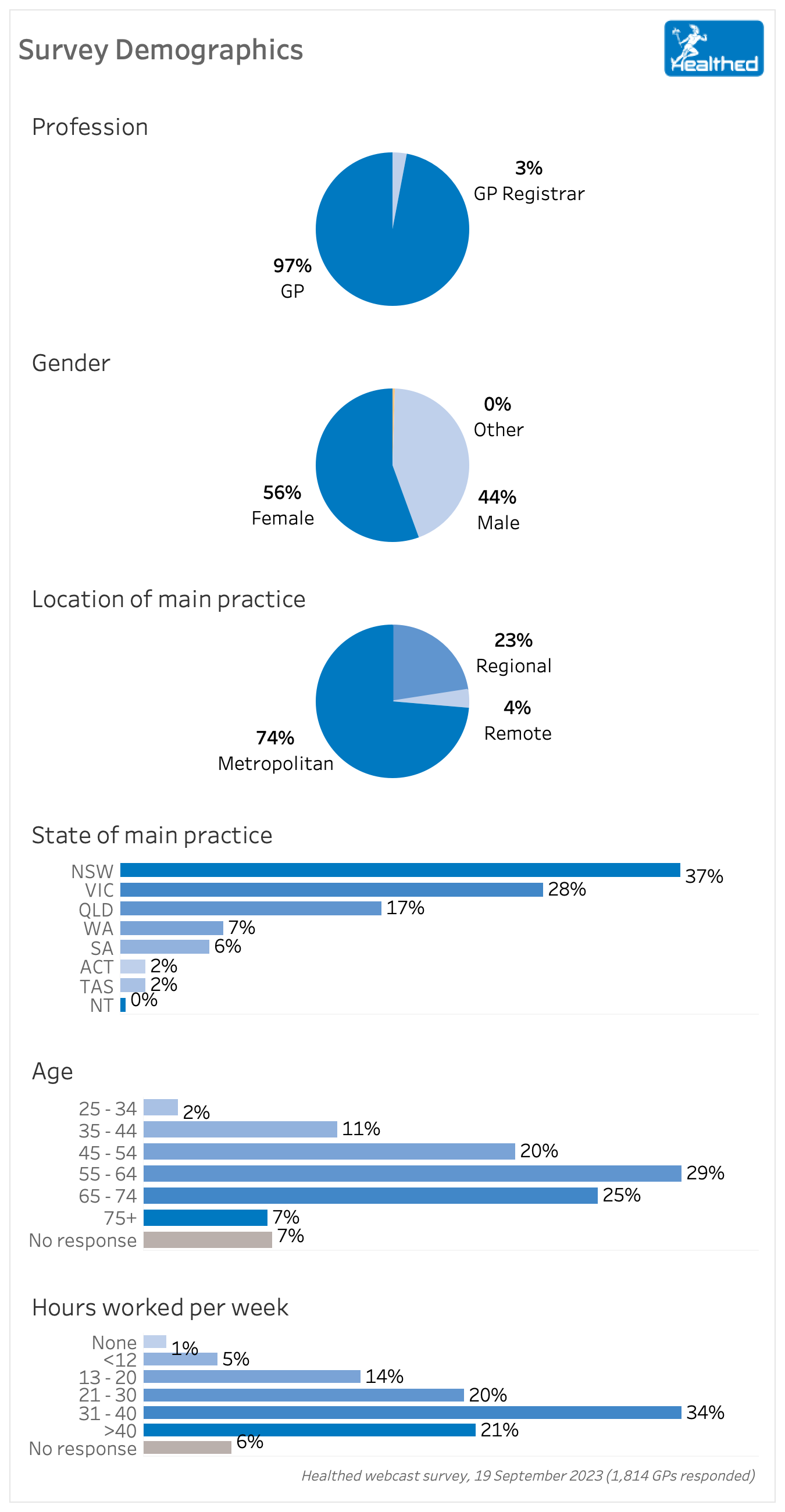
International medical graduates (IMGs) make up half of the Australian GP workforce, yet they commonly experience discrimination, both from patients and colleagues, according to Healthed’s national survey of more than 1800 GPs.
More than one third (37%) of IMGs report experiencing racial/ethnic discrimination from patients in the past 5 years, compared to just under one fifth (17%) of Australian medical graduates (AMGs).
Perhaps of greater concern, more than one quarter (26%) of IMGs report experiences of racial/ethnic discrimination from colleagues in the past 5 years, while one in ten AMGs report the same experience.
These experiences are likely to be an additional contributor to burn out, with serious workforce implications — yet the RACGP has remained silent on the survey findings, despite repeated requests for comment.
Our survey did not differentiate ethnic background of the Australian graduates, but respondents were split 50/50 between those with Australian and international qualifications, which roughly reflects the overall GP workforce.
Clinical Professor Leanne Rowe, who co-authored the book “Every Doctor: healthier doctors = healthier patients,” said we’ve been hearing about discrimination in the medical profession for decades, and the lack of progress is “completely unacceptable.”
“The results of the Healthed survey are unfortunately in line with other reports on unacceptable discrimination and racism in medicine,” Professor Rowe said.
“As a profession, I think we need to question why are we not cutting through on these serious issues, and how we can change the status quo.” – Professor Rowe
“The AMA and our Colleges need to take a stronger stance,” she continued.
“People often say they have a zero-tolerance approach, but when they come to implement their policies, if they have them, their response is lacking. The medical profession must come into line with contemporary thinking and compliance on HR issues and workplace health and safety.”
Dr Mukesh Haikerwal, deputy chair of Australian GP Alliance, and a Melbourne GP who originally trained in the UK, agreed that the problem is longstanding.
He recalled that when he called out discrimination in 2005 as AMA president, “the interesting thing was that many Australian graduates had ‘different’ names or looked ‘different’ and felt at the time very vulnerable and discriminated against.”
“There was some protection from this with a degree from a ‘respected’ jurisdiction, but from patients (and some ‘colleagues’) it was the immediate what you looked like, how you sounded and what your name was. Some changed their surnames,” Dr Haikerwal said.
Professor Rowe said bad behaviour from patients should not be tolerated. “This is a whole of practice issue, where everyone should be empowered to educate patients on acceptable and unacceptable behaviours for the psychological safety for all.”
When it comes to discrimination that IMGs attributed specifically to their having trained overseas, 38% of surveyed IMGs said they had experienced it from colleagues, and 28% from management or employers.
There was no meaningful difference between responses from GPs working in rural or regional areas compared to those working in metro areas.
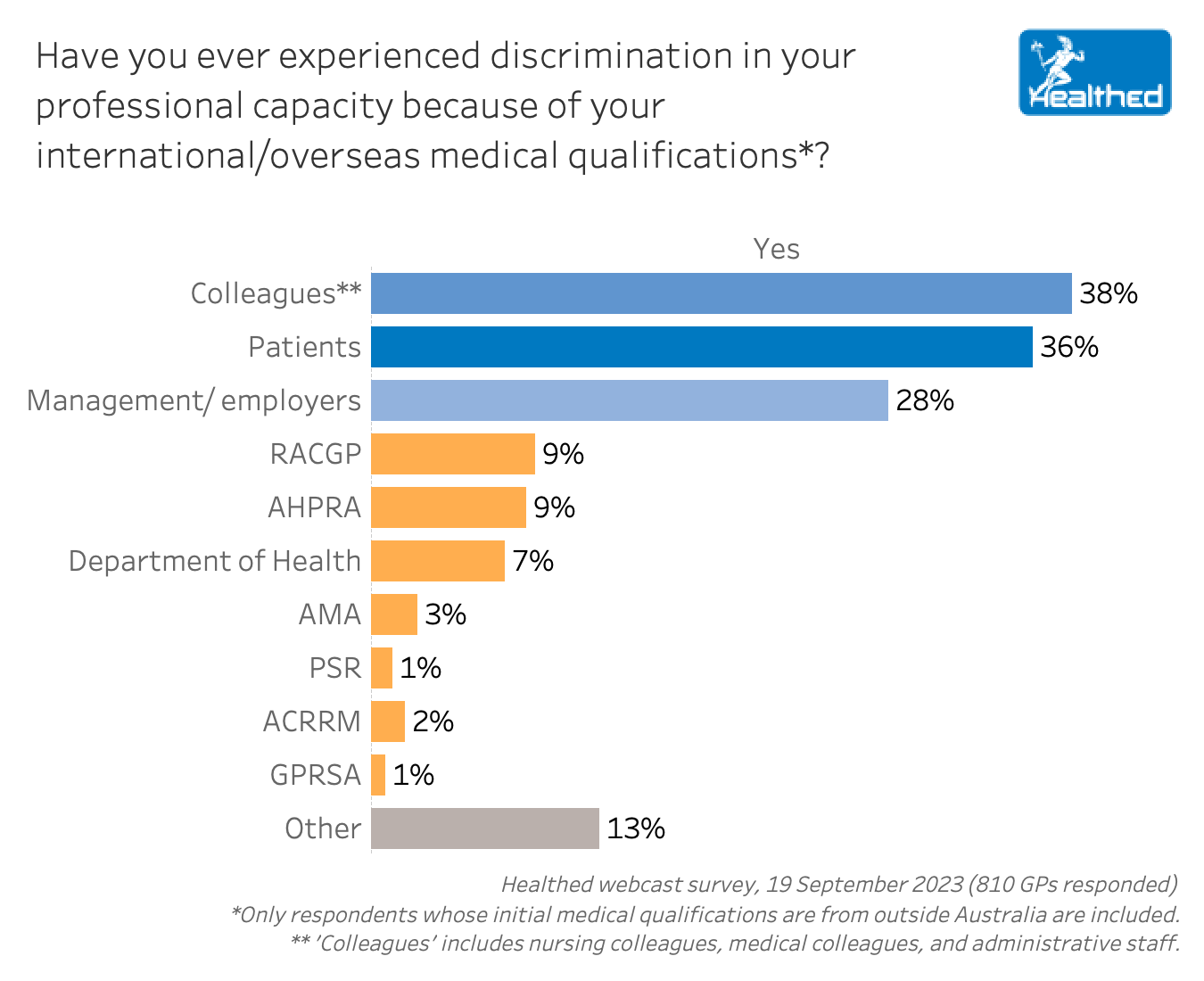
Although it was much less common for doctors in general to say they had experienced racial or ethnic discrimination from organisations or peak bodies (e.g. AHPRA, RACGP etc.) in the past five years, 16% of IMGs said they’d experienced it because of their international qualifications.
Despite all this, more than three quarters of Healthed survey respondents agreed that doctors who received their initial medical qualifications overseas are generally treated with the appropriate level of respect from their professional community—with international medical graduates more likely to strongly agree than Australian-qualified GPs (15% compared to 10%).
Dr Haikerwal was not surprised. “This is what I would expect – not wanting to trash the system you have chosen to work in,” he said.
One of our GP editors commented on a recent gaffe by the RACGP, which saw the College grovelling and promising to change.
“I’m a GP of ethnic origin. A few weeks ago we all received a long email from the president where she publicly apologised for omitting the names of two IMGs from a photo caption. In that email she committed the College to tackling racial discrimination. To many GPs with a similar background to mine, that was a brief moment of public self-flagellation and virtue signalling, which seemed to be nothing more than a cringy expression of white guilt,” they said.
“Isolated and sporadic gestures like that are not going to help us reduce the experience and impacts of racial discrimination in medicine, but they are useful for short term anaesthesia and memory loss. Like many of my colleagues with non-anglo ethnic backgrounds, I am keen to see what the College does now that this survey has been brought to their attention.”

RSV Prevention in Infants and Pregnant Women

STIs – Common and Tricky Cases

Role of Testosterone During Menopause - Evidence vs Hype

Vision and Driving Fitness: Key Insights for Health Practitioners
Yes
No
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
