Articles / More prescribing powers for nurse practitioners?

GPs are wary of the expanding role of nurse practitioners and endorsed midwives, who may soon be able to prescribe PBS-listed medicines completely independently, if draft laws tabled in parliament late last month succeed.
In a speech announcing the draft legislation, Assistant Minister for Health and Aged Care Ged Kearney said the skills and time of nurse practitioners and endorsed midwives were being “disrespected.” Moreover, the current legislative requirement for a ‘collaborative arrangement’ with a doctor creates barriers to accessing care, she added.
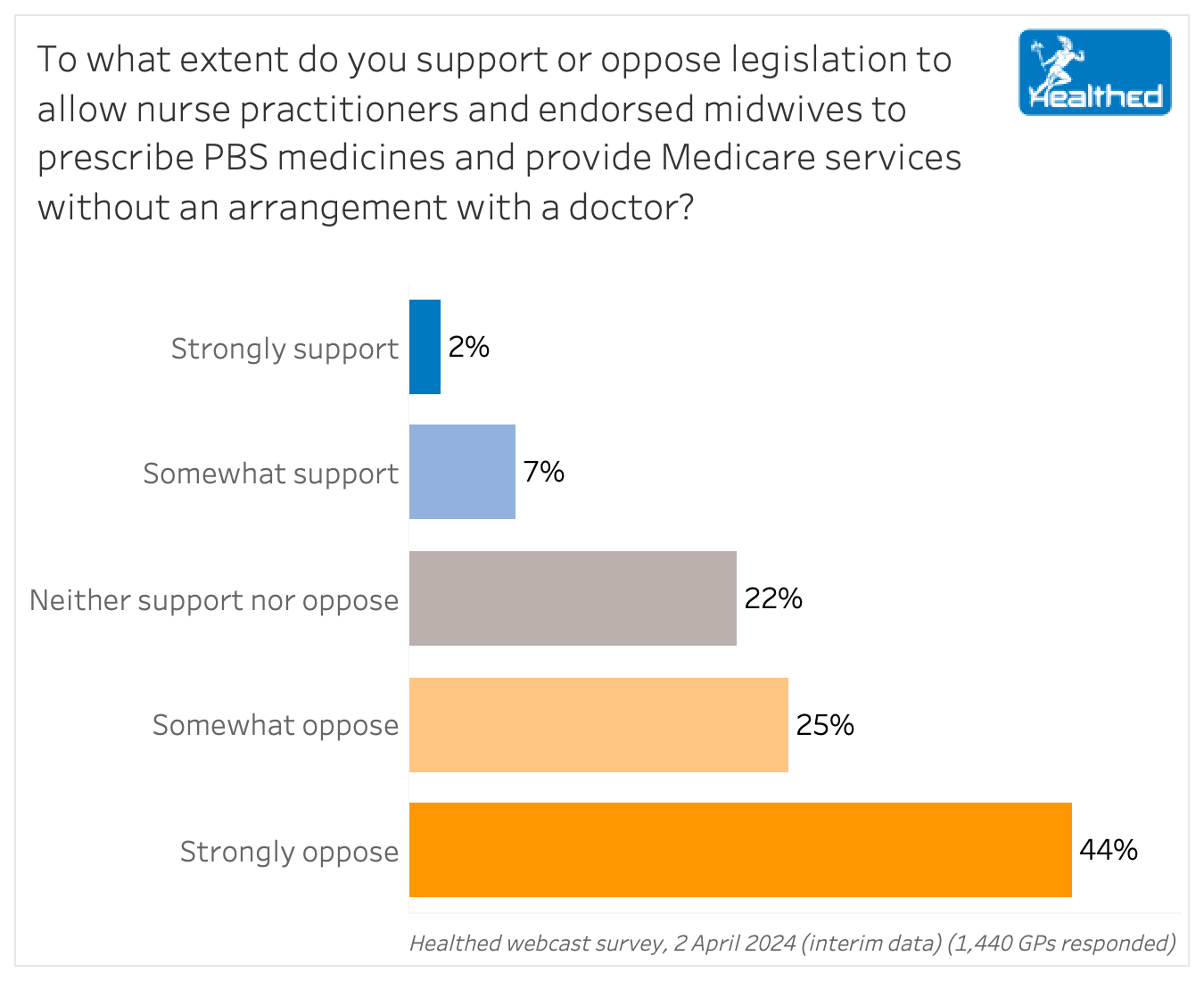
When asked directly for their views on the legislation that would allow nurse practitioners and endorsed midwives to prescribe PBS medicines and provide Medicare services without an arrangement with a doctor, 69% of GPs said they opposed it.
Interim results from Healthed’s most recent survey suggest 51% of GPs think the current protocol effectively uses the skills of these health professionals. But 32% were on the fence, and 17% felt the current requirements were a poor use of their skills.
Just 20% of more than 1400 GPs who responded so far believed that the collaborative arrangements currently in place create barriers to patient care— while 34% had no opinion, and the remaining 46% disagreed with that premise.
Assistant Minister Kearney, herself a nurse, argued that removing the requirement would not impede on clinical collaboration or the delivery of care.
“These health professionals are already regulated by the professional standards for practice and quality and safety guidelines issued by the Nursing and Midwifery Board of Australia, which require collaboration with other health professionals,” she said.
In free text comments, many GPs raised concerns about lack of adequate training, potential patient safety risks due to knowledge gaps, and the need for doctor supervision.
“Whilst Nurse Practitioners and endorsed midwives are excellent health care professionals, they have limited scope of knowledge… It’s important for a doctor who has more experience to oversee their suggestions,” one GP said, in a view echoed by many.
“This is the slippery slope. Responding to a doctor shortage by using non-doctors to work as doctors increase risk of harm to patients. Better to encourage them to study medicine instead.” – surveyed GP
Doctors also worried about increasingly fragmented care.
“Fragmenting medical practice is the ‘cheapskate’ alternative to training enough doctors. It is also begging severe adverse outcomes… Let’s progress towards integrated, cooperative, respectful professional teams dealing with patient health, not fragmentary political quick fixes!” is how one doctor put it.
Many GPs in Healthed’s survey do support nurses with specialised training being able to independently prescribe some medications, particularly for problems they encounter regularly.
“I would support a trial of NPs prescribing independently if the range of medications prescribed are those with clear prescribing guidelines. I would like to see mutual respect for the skills of both doctors and NPs,” one surveyed GP said.
“Nurse practitioners practice in their own very limited field. Autonomous prescribing should be limited to their field of expertise only, and provided drug interactions and relevant co morbidities are well understood. I would feel more comfortable with a two-way discussion and knowledge exchange with a nurse and appropriate doctor who work well as a team.” – surveyed GP
“If their personal liability insurance will cover them for prescribing, and they are trained to do so, it should not be a problem. Coming from the US where nurse practitioners own their own practices, they contribute to health care within their own scope of practice and are under the same guidelines as prescribing doctors,” another GP noted.
Other comments suggested that the changed legislation could particularly benefit those in rural and remote areas, and noted that nurses and midwives could, and likely would, still call on doctors as needed:
“Competent well-motivated nurses know when to involve a doctor and the limits of their own knowledge, in the same way as competent and well-motivated GPs know when to involve a specialist.”
“There are clearly situations, and some medications, in which unsupervised nurse prescribing is appropriate and necessary. However, I think medical oversight or consultation if available, is usually wise.”
“Our health system is under great pressure, and getting support from experienced nurses or midwives will help in better patient care and management, but this requires close collaboration with a GP who is aware of the patient’s medical history and social situation.”
“I have only worked with practice nurses who provide a good level of care to my patients in a cooperative way. We have mutual respect for each other…There are many presentations which can easily be managed by NPs as with other health providers who independently provide services under Medicare.”
“Midwives and nurse practitioners are trained professionals providing health care where medical doctor may be absent. Most of these professionals are aware of their scope and will seek further advice when needed. Where clear guidelines exist, it should be reasonable to allow these professionals to work and prescribe independently.”

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart

Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
