Articles / Three problems with the bulk billing incentive

The tripled bulk billing incentive came into effect on Wednesday — welcomed in with glowing media reports and peak bodies singing its praises. The RACGP said it “will help slow the decline in bulk billing for vulnerable patients and relieve pressure on hospitals,” while the AMA said it provided “much needed cost-of-living relief for millions of Australians” and signified “the government’s real commitment to providing more support for patients who need to see a GP.”
The incentive payments apply when medical practitioners bulk bill children under the age of 16, as well as patients with a concession card. The payments have increased to between $20.65 in metro areas and $39.70 in remote areas.
So will the policy result in better access to care for those who need it most, or improve the financial viability of GPs practices?
Dr Chris Irwin, president of the Australian Society of General Practice, contends that it will help in rural areas, where the increase is significant. But metro areas are another story.
“In metro areas I do not think it is anywhere near enough to fund high quality care,” Dr Irwin said.
“I think this decision to slightly increase metro incentives—and the fanfare of the government and the RACGP hailing this as a ‘gamechanger’ — will put more unnecessary stress on doctors who will agonise over taking a $30-40 loss on each bulk billed metro patient — versus billing appropriately and worrying about their patient’s access to care.”
Healthed’s survey data — and indeed the RACGP’s own polling — lends support to Dr Irwin’s view. More than 80% of surveyed GPs told Healthed they would not be changing their bulk billing after the policy was announced in May. As of 4 November, 73% of respondents to NewsGP’s weekly poll said their practice would not be changing their approach to billing with the start of the increased incentives — a further 10% said they were unsure.
In free text responses to Healthed’s 31 October survey, many GPs said it would not change their billing patterns.
“It is not nearly enough to make me consider bulk billing. My lease payments rocketed this year, I am barely breaking even,” one GP said.
“Too little too late,” said another. “Rather than reimbursing us fairly years ago to entice doctors to become GPs, everything is 15 years too late.”
“By saying this was a major win, the College is buying into the government spin and thus is perversely contributing to the already unreasonable pressure on doctors to bulk bill even when they can’t afford to,” another GP said.
“This budget is not a ‘gamechanger’ for GPs or their patients — it is a cynical ploy by health bureaucrats to figure out the minimum extra funding necessary to make doctors grumble a little, but still bulk bill.” Dr Chris Irwin
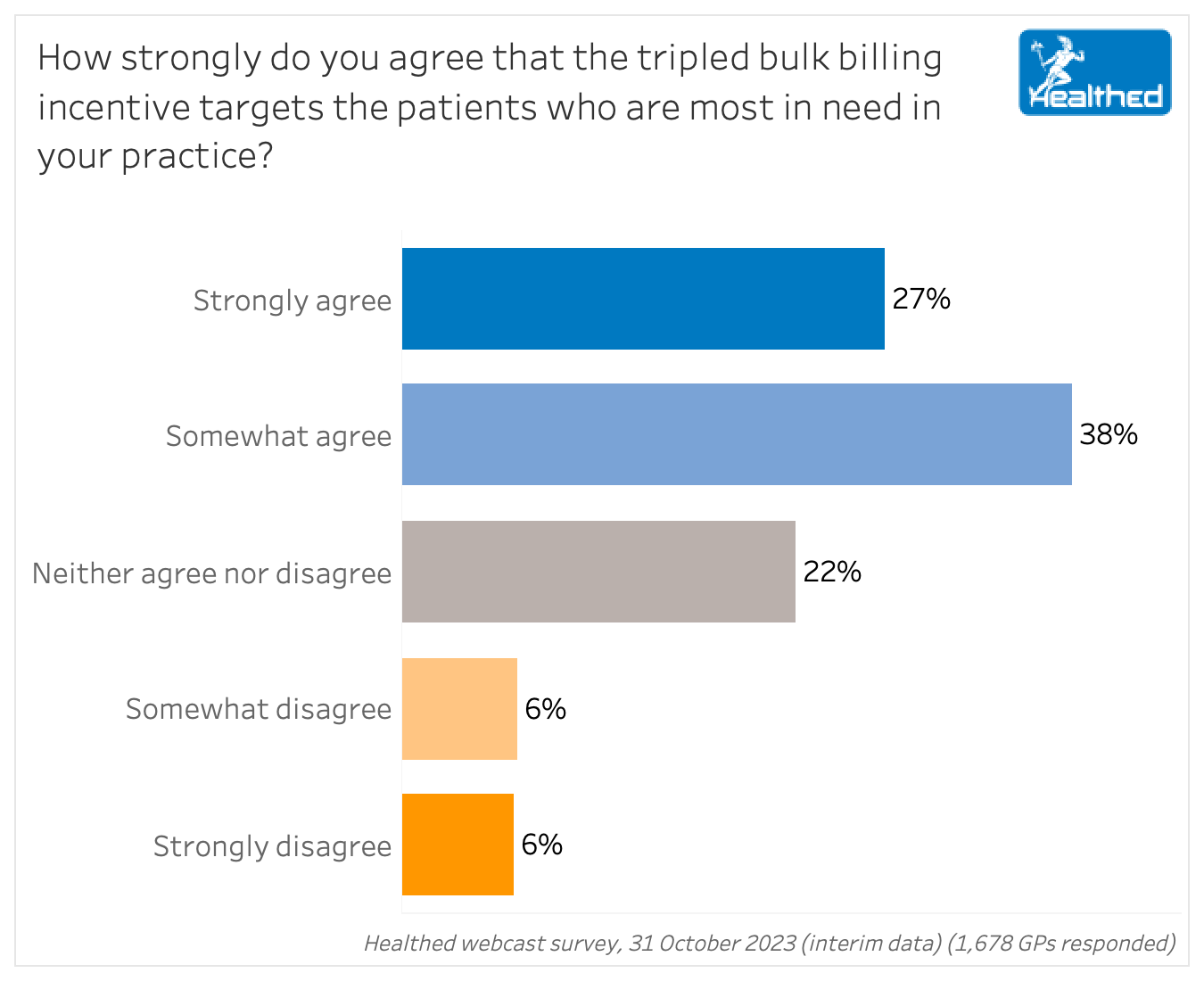
In Healthed’s latest survey, just over a quarter of almost 1700 GP respondents strongly agreed that the incentive targets those most in need in their practice — while 38% said they “somewhat agree.” Another 22% of GPs were on the fence, and 12% disagreed that their most vulnerable patients would benefit. In free text comments, GPs identified many gaps.
Many surveyed GPs said patients with mental illness, as well as those with other chronic and complex conditions and comorbidities that require frequent visits or longer consultations, should be eligible for the bulk billing incentive. Many also noted that low-income patients who don’t have concession cards, for various reasons, would slip through the cracks.
“It misses those on minimal incomes who already miss out on the concession card and all its benefits.”
“Some low-income families with children and single parent families who are not eligible for commonwealth concession card struggle to pay full fee and may not seek medical help when needed due to financial restraint,” one GP explained.
“This gives very little assistance to people struggling just over the threshold for a healthcare or concession card, and there are lots of those,” said another.
“No help with mental health consultations which are increasing in frequency and complexity and time consumed for limited remuneration,” another wrote.
Meanwhile, affluent parents with kids under 16, or asset-rich retirees would be eligible for the bulk-billing incentive. “I have patients who live with Sydney Harbour views, with concession cards,” one GP noted.
About one quarter of survey respondents said the incentives should increase for everyone.
When asked which additional groups should be eligible, one surveyed GP said: “All patients with a Medicare card – no one should be worried about not being able to pay to see a GP when they need to.”
“I feel government should offer, rather than solely bulk billing incentives, increased patient rebates for ALL patients as many are under financial distress and will receive no benefit from the current plan.”
“Madness that it doesn’t cover mental health consultations — another fiscal blow for women GPs and failure to recognise that we tackle more of the complex GP consults, examine patients more and do more mental health,” one GP in Healthed’s most recent survey noted.
“This greatly benefits corporate 6 min practitioners, and is a political stunt. It adds very little to my 40-60 minute consultations, and indeed it is an insult to caring GPs,” another surveyed GP said.
Dr Irwin agreed, noting that having the same rate, regardless of consult length, was another major flaw.
“This once again entrenches short visits and suboptimal healthcare. Healthcare shouldn’t be funded less because a patient is vulnerable and complex — but it is currently because the rebates are worth less than half of what it actually costs to provide good medical care,” he said.
Survey analysis and visualisation – Yasmin Clarke
Survey conception and design – Dr Ramesh Manocha, Yasmin Clarke and Lynnette Hoffman

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart


Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
