Articles / Why are so many Aussies on antidepressants for so long?

Australia has one of the highest rates of antidepressant use in the world, with one in seven Australian adults taking them—and that number is continuing to rise.
The increased use is largely because people are failing to stop antidepressants, according to Professor Katharine Wallis, Head of the Mayne Academy of General Practice at the University of Queensland Medical School, and lead of the RELEASE (REdressing Long-tErm Antidepressant uSE in general practice) study.
While the recommended duration for antidepressants is 6 – 12 months, the most recent figures show Australians are taking them for an average of four years, Professor Wallis said.
Moreover, she suspects these figures – which her team are in the process of updating – are probably worse now, because “use, we know, is going up.”
According to recent data from the Australian Institute of Health and Welfare, GPs prescribe 92% of antidepressants.
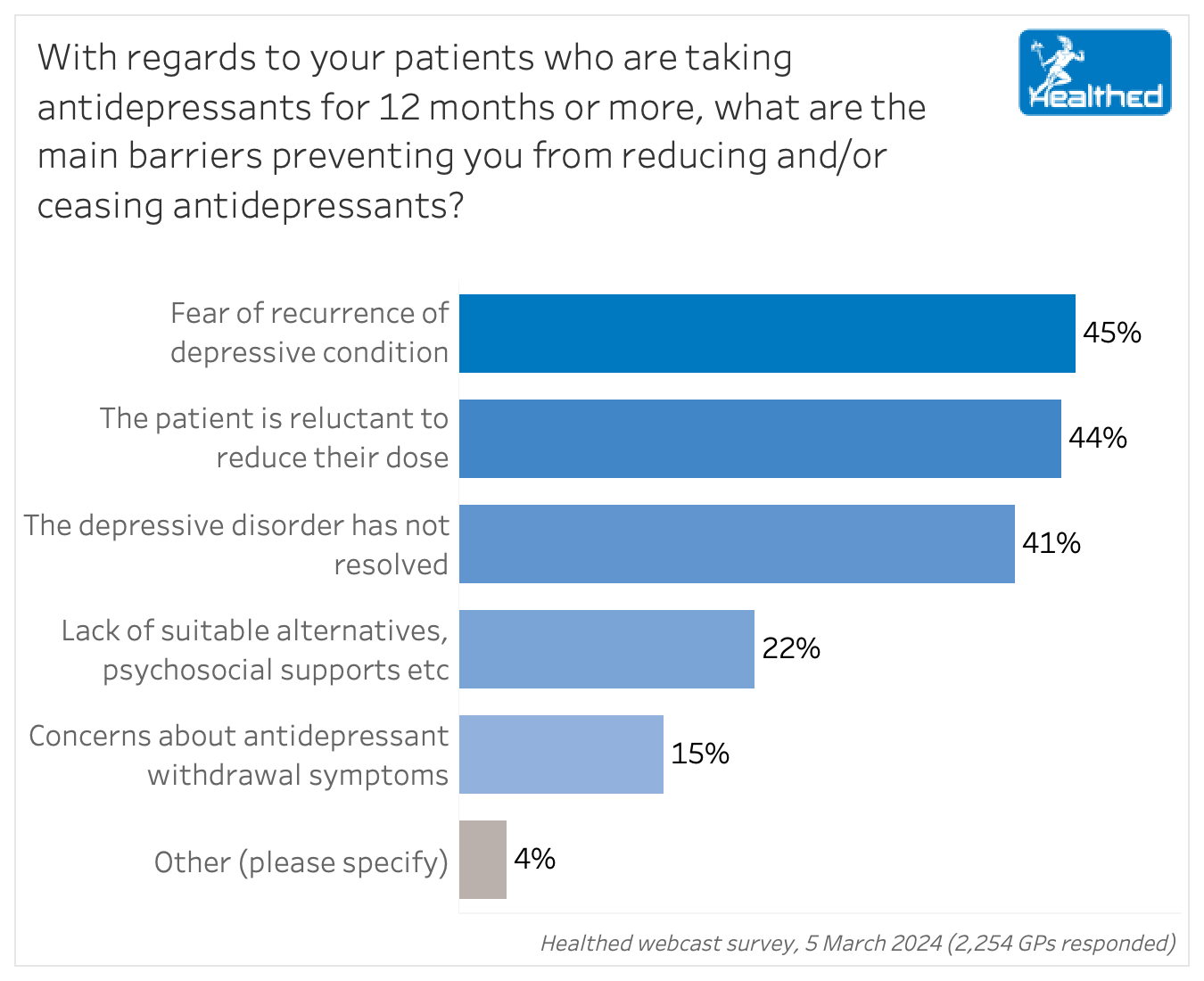
Qualitative research by Professor Wallis’s team has found patients expect their doctor to tell them when to stop — but Healthed’s 5 March survey of more than 2200 GPs has identified some key barriers to deprescribing.
Fear of recurrence and patient reluctance to reduce their dose topped the list, cited by 45% and 44% of respondents respectively (more than one response could be chosen).
Dr Mark Horowitz, co-author of the just-released Maudsley Deprescribing Guidelines, said the idea that depression is caused by low serotonin has persisted despite lack of evidence, and this belief predicts patients’ unwillingness to stop medication.
“This needs to be actively countered,” Dr Horowitz said in a public lecture hosted by the Australian Society for Psychological Medicine on Tuesday night.
Past bad experiences when stopping (often very quickly) are another barrier, “especially when withdrawal effects on stopping are interpreted as relapse and an indication that they need the drug to stay well,” Dr Horowitz added.
Professor Wallis said both patients and doctors confuse withdrawal symptoms with recurrence, and Healthed’s survey found 48% of GP respondents were either only ‘somewhat confident’ or ‘not at all confident’ in their ability to distinguish between the clinical features of withdrawal versus recurrence.
While fear of relapse is a legitimate concern for those with recurrent conditions, Dr Horowitz pointed out that many people start antidepressants because of a specific stressor, and stay on them long afterward.
To that point, Professor Wallis noted that antidepressants don’t solve underlying social issues — but are more commonly prescribed in low socioeconomic areas.
“A lot of people struggle with life – feeling down or distressed or anxious – and if we had a magic pill people could take to instantly feel better that would be great. Unfortunately, we know that prescribing of these drugs is more common in areas where there is more socioeconomic deprivation, and we know that the drugs can’t treat grief or homelessness or unemployment or divorce or all the other reasons people start taking them,” Professor Wallis said.
In situations like these, she said GPs can recommend strategies such as exercise, social connection and talking therapies. “In the long run, those things are likely to be more effective at supporting change.”
More than 40% of Healthed’s survey respondents also said lack of symptom resolution was a barrier to antidepressant cessation.
Professor Wallis said that if symptoms have persisted for a year, it’s evidence that change is needed.
“If you’ve been on these drugs 12 months and you’ve still got symptoms, it tends to suggest that the drugs are not working, so why keep taking them?”
According to the Therapeutic Guidelines, people don’t always respond to the first antidepressant, and a trial of more than one is often needed to achieve an acceptable response. In cases where the patient doesn’t respond to an antidepressant, the TG also recommends considering whether:
Dr Horowitz said there are several reasons to deprescribe: the medication may no longer be needed, the stressor may have resolved, the patient may have developed alternative coping mechanisms or they may wish to try a different strategy—to name a few.
Common adverse effects of antidepressants include sexual dysfunction, emotional numbing, fatigue, impaired memory and concentration; so stopping antidepressants when they are no longer needed can improve quality of life, he added.
Additionally, antidepressant use is associated with increased risk of strokes, obesity, osteoporosis, falls, cardiovascular disease and premature mortality, according to long term observational data Dr Horowitz cited.
In older adults where polypharmacy is common, deprescribing can also help reduce the associated risks.
Professor Wallis recommends reviewing whether patients still need antidepressants every time you write a repeat prescription, although she notes this can be tricky, especially when pressed for time.
“Save prescribing of any drugs for the pointy end – for people with really severe problems, which is not the majority of people in general practice we’re seeing … Only a small proportion would be at the pointy end, so we probably are prescribing to too many people,” Professor Wallis added.
Stay tuned for more articles on how to safely deprescribe, and how to tell the difference between withdrawal symptoms and recurrence.

An Update on Heart Failure in Primary Care

Allergen Introduction – Practical Tips for GPs

Falls Prevention – A Practical, Evidence-Based Update on What Really Works

Vulvovaginal Health – From Childhood to Menopause

Very overestimated
Moderately/slightly overestimated
Quite accurate
Moderately/slightly underestimated
Very underestimated
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
