Articles / ADHD survey: most GPs unlikely to manage more ADHD patients

While most general practitioners favour expanding GPs’ powers to formally diagnose ADHD, at least for those with special training, the majority wouldn’t choose to diagnose or treat more of these patients, a Healthed survey of more than 1300 GPs has found.
The survey follows the release of a Senate Inquiry report in November which recommended that GPs with appropriate, accredited education and training should be able to play a greater role in the identification and support of ADHD.
“GPs appear well positioned to expand their role as it relates to ADHD management, particularly in the co-management and co-prescribing of medications to support people with ADHD,” the report stated.
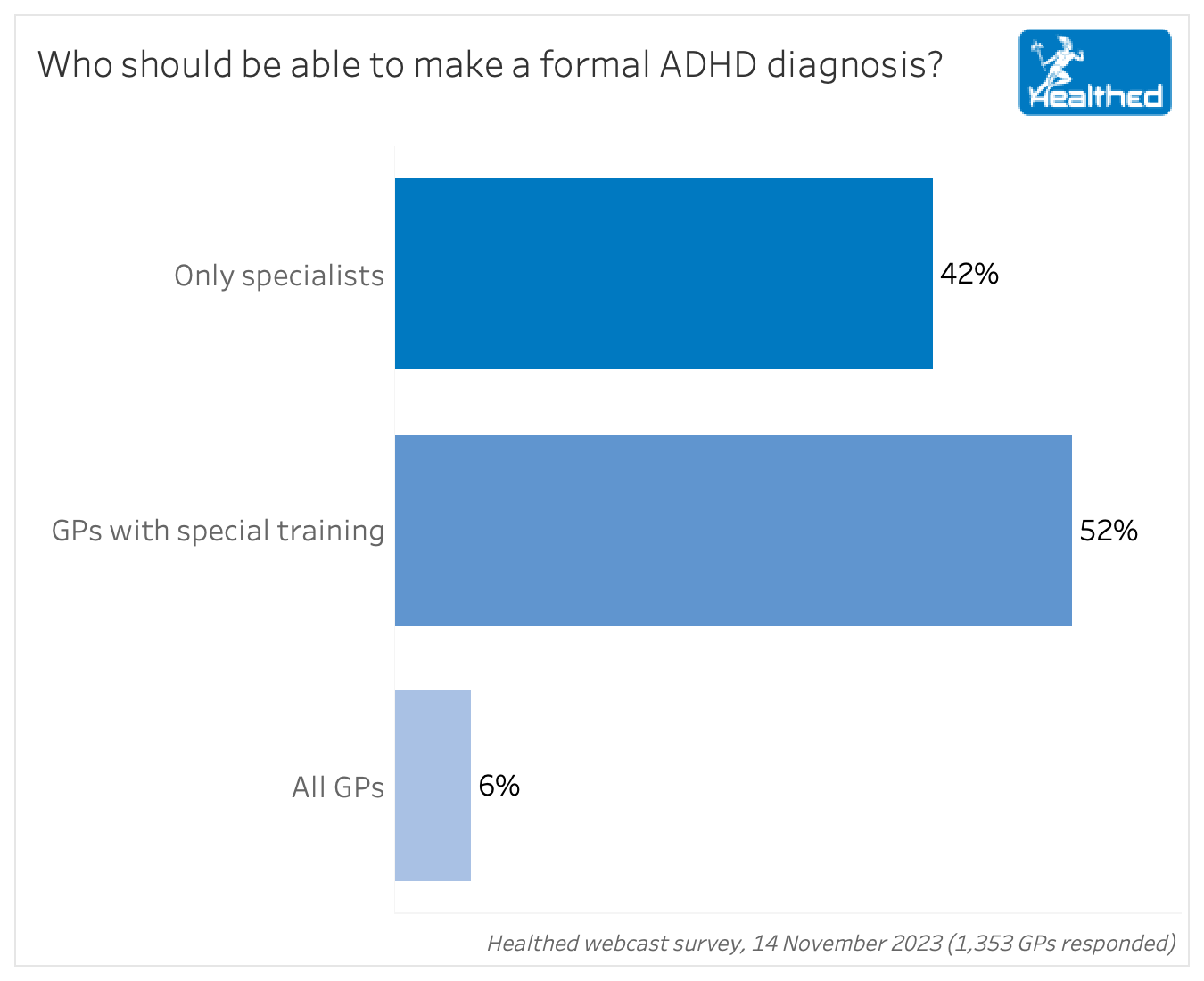
A significant minority (42%) of GPs in Healthed’s survey said only specialists should be able to make a formal ADHD diagnosis, while 6% said all GPs should be able to. The remainder supported allowing GPs who undergo more specific training to diagnose the condition.
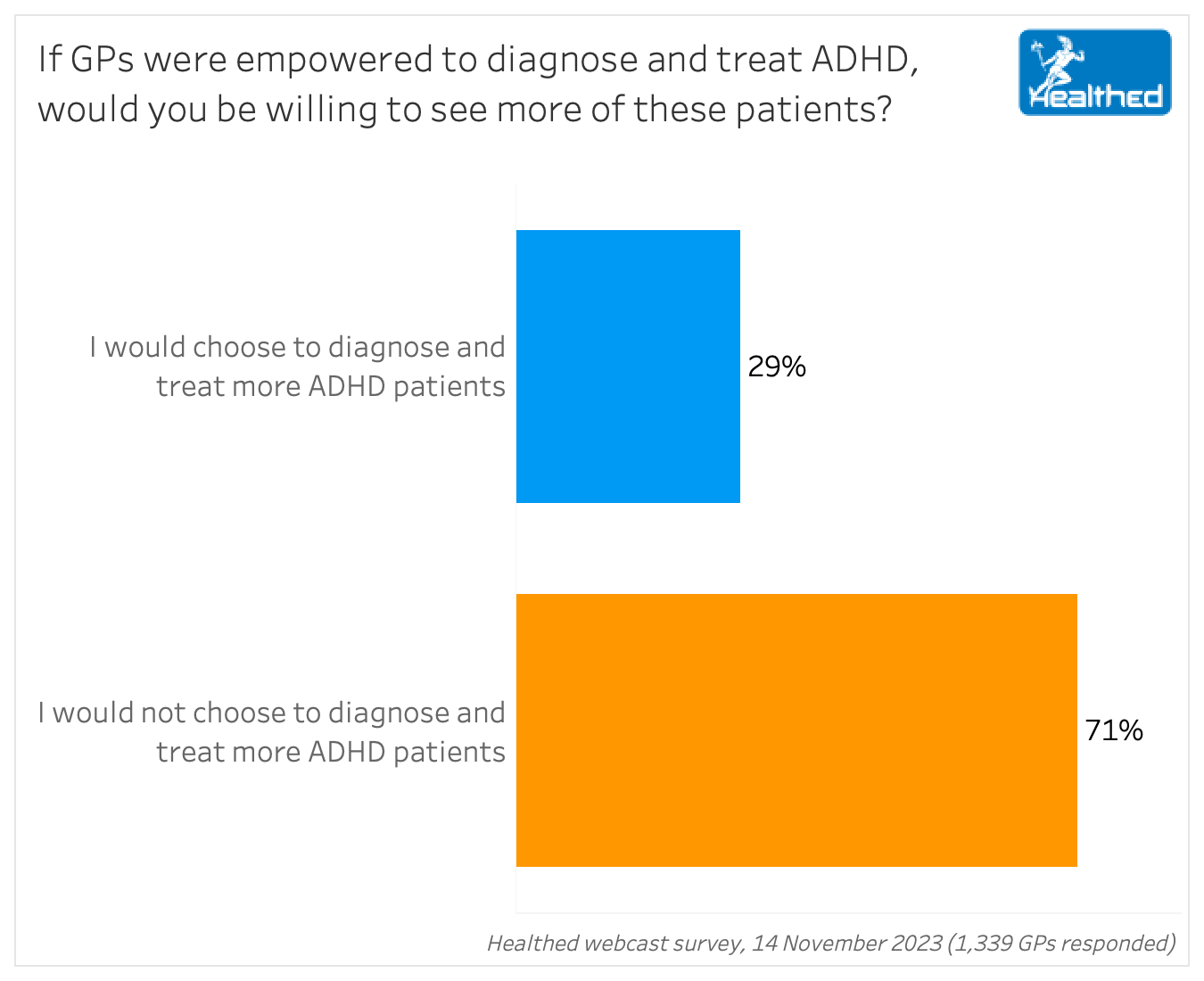
Well over two thirds of GPs said they would not choose to diagnose or treat more ADHD patients if given the option — with just 29% saying they would.
The survey also looked at GPs confidence levels when it comes to making an ADHD diagnosis:
Dr Karen Spielman, a GP with a special interest in mental health, who is on the board of the Australian Society of Psychological Medicine, said there’s a couple of factors likely at play. For one thing, levels of interest and expertise vary widely.
“Some of us are really interested and have upskilled and can manage to a higher level than others who have little interest or desire,” she said.
But perhaps even more significantly, increased funding for longer consultations and higher Medicare rebates for mental health consultations might help change the calculation for many GPs, Dr Spielman said.
“The Medicare system is so slanted towards quick appointments these days, there’s so much pressure to make a quick diagnosis and a quick referral. And I think that’s really counterproductive,” she said.
This was echoed by some GPs in the free text responses.
“GP land is not funded to provide this avenue – these consults would take considerable time to do correctly, with collateral reports etc from psychologists, schools, allied health teams,” one surveyed GP commented.
Another surveyed GP said the decision to diagnose and treat more ADHD patients would “depend on the training and the Medicare rebate for doing this work as compared to a psychiatrist.”
However Dr Alison Poulton, a paediatrician and senior lecturer at the University of Sydney who specialises in ADHD, said even a small proportion of GPs working in this area could make a tangible difference.
“It’s actually really encouraging that there are 3% of GPs who feel that they are quite informed about ADHD,” Dr Poulton said, adding that this might be further increased if GPs are adequately supported and given additional training to actively diagnose and treat ADHD. “Because there aren’t enough of us specialists to meet the need for ADHD, and that was very clear in the report from the Senate Inquiry.”
There may be even more scope for GPs when it comes to co-managing patients already diagnosed with ADHD, she added.
“The main bottleneck is in prescribing. So specialists are under pressure to prescribe medication to as many of the patients who need it as possible, but if they can leave the rest of the picture to the GP – who knows the family, and can do a mental health care plan, refer to a psychologist, that kind of thing – then that’s going to be really helpful,” Dr Poulton said.
“GPs, by definition, have a holistic view of the patient and their family,” she continued.
Dr Poulton is currently working on a pilot study at Cranebrook Community Health Centre which is training GPs to diagnose and treat children with ADHD in their GPs clinics. To do this, they attend 12 training sessions, plus additional coursework. Since September two GPS have been trained and are running an ADHD clinic in their practice, she said.
Though many GPs in Healthed’s survey said they already felt too stretched, or wouldn’t feel comfortable without extensive training and experience, others said they would embrace the opportunity.
“With the correct training, I would gladly see more of these patients,” one GP said.
“As GPs, we know our patients over years (typically these specialists meet them for hours). We are able to access exactly the same tools these specialists utilise to diagnose ADHD, we are expected to continue to monitor and prescribe medications, and otherwise manage our ADHD patients…”
“Why should we be expected to do additional training courses to simply provide care to our patients and utilise tools/resources that we can already access, but are not apparently “qualified” to apply? It’s an insult.”
“Medications to treat ADHD are S8 and hence need authority. To cover oneself from potential medical board issues or HCCC complaint, I would steer clear.”
“I would be happy to see my patients as part of their care, but wouldn’t want to be seeing new patients and primarily doing this.”
“I’m already too busy and I imagine it would be a very time intensive process.”

Menopausal Hormone Therapy - What Dose of Estrogen is Best?

Cardiovascular Benefits of GLP1s – New Evidence

Oral Contraceptive Pill in Teens

RSV and the Heart



Modified but kept in place
Eliminated entirely without replacement
Maintained as is
Completely replaced with an alternative system
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
